Background: Pregnant women were more susceptible to greater mortality and morbidity rates when compared to general population in the previous SARS and H1N1 pandemics. Many studies have been published about effects and outcomes of COVID-19 in general population. Limited data is available on COVID-19 in pregnancy. Our objective is to characterize clinical features, maternal and fetal outcomes of hospitalized SARs-CoV2 PCR positive pregnant women during the peak of the pandemic.
Methods: This is a retrospective single-center descriptive study. All pregnant women with SARS-CoV2 positive PCR admitted to Lincoln Hospital between March to July 2020 were included in the study. A detailed review of medical records was performed and the baseline characteristics, clinical features, clinical course including maternal and fetal outcomes were evaluated. Categorical variables were characterized frequency (%) and continuous variables as median with 25-75 IQR.
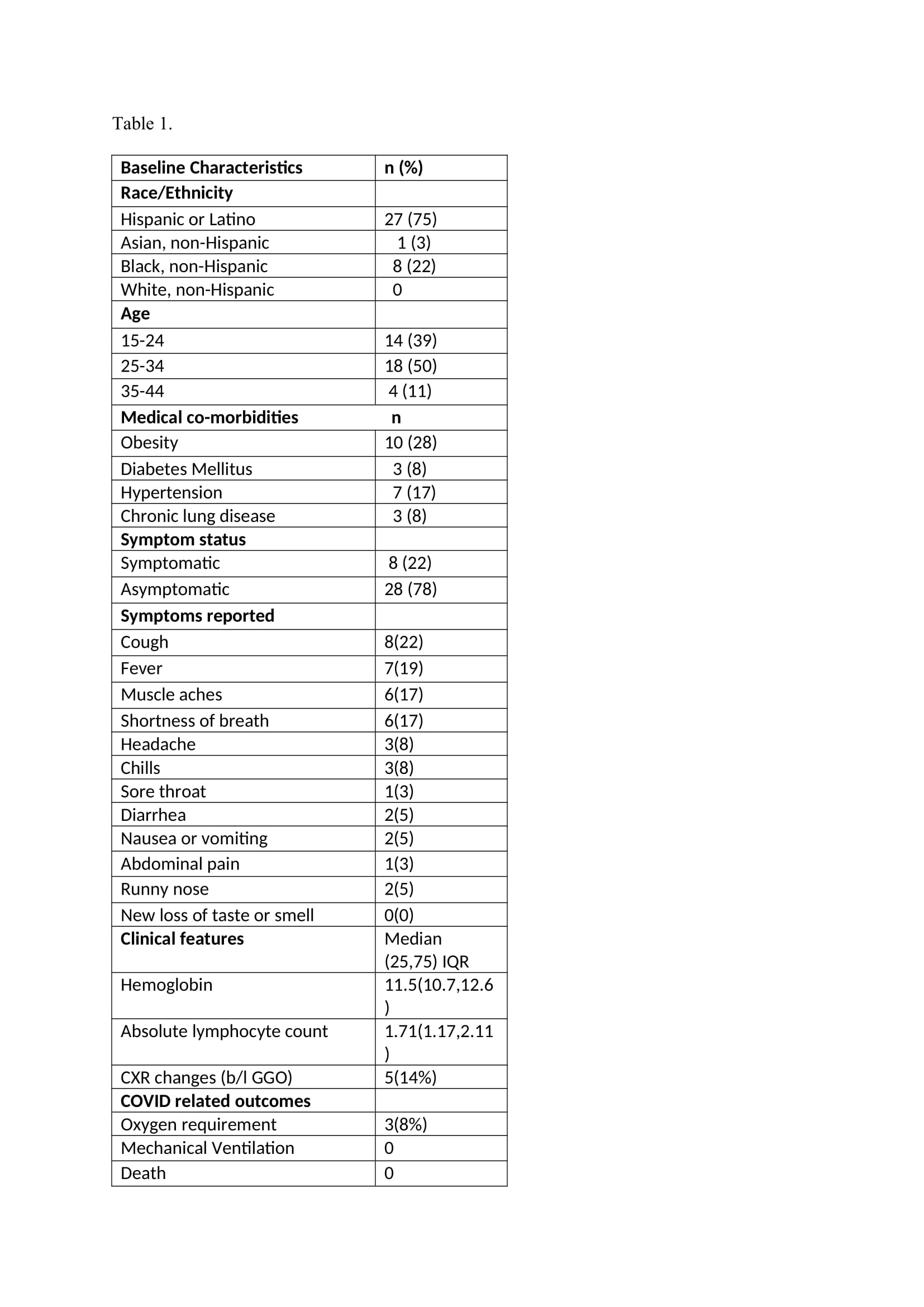
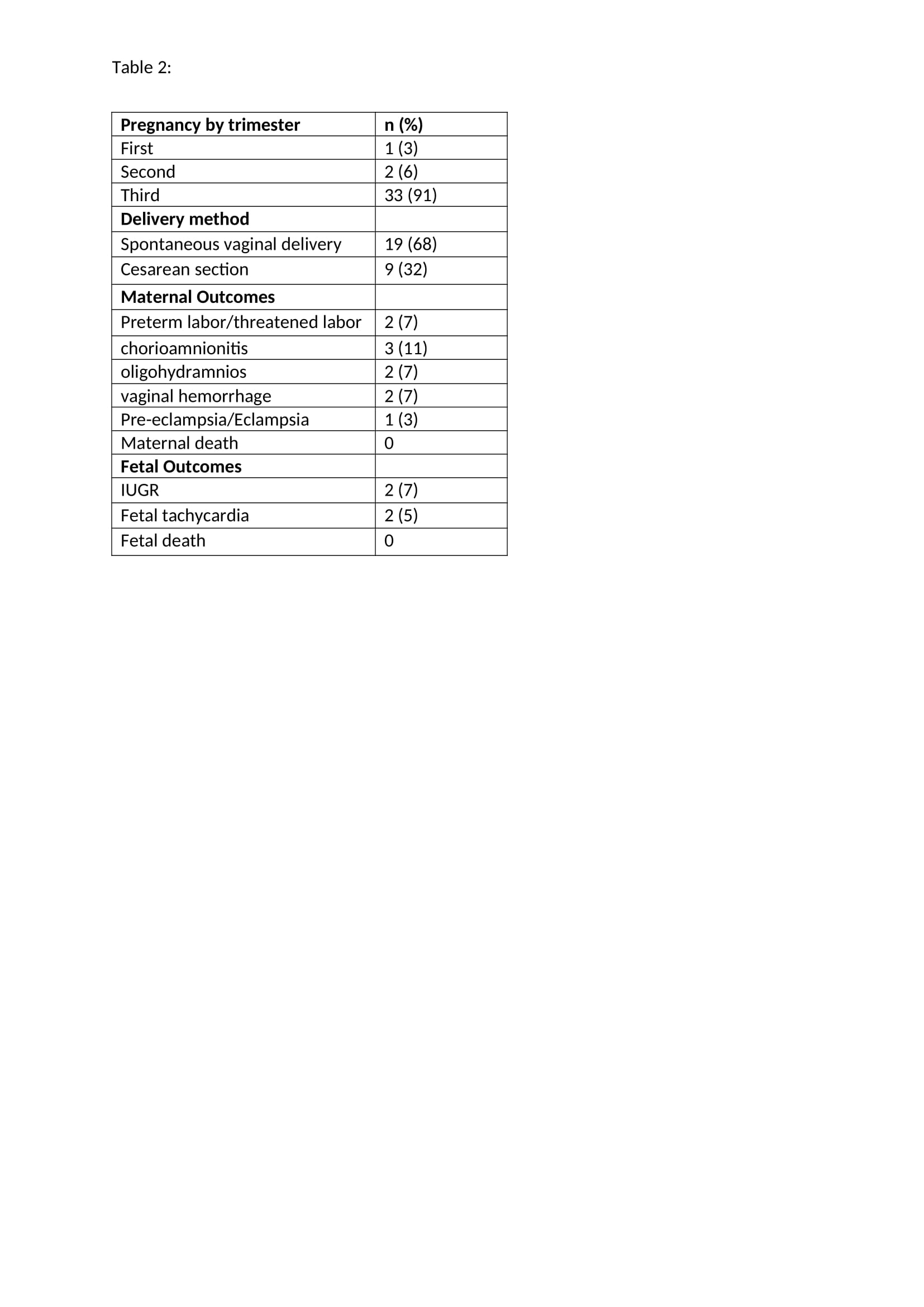
Results: Thirty-six SARs-CoV2 PCR positive pregnant women were admitted during the study period. Baseline characteristics are described in table 1. 75% were Hispanic, 22% were African American, 2.7% were Asian. 78% of the pregnant women did not have any symptoms of COVID-19 infection, while 22 % were symptomatic of which 14% had features of COVID-19 pneumonia confirmed on X Ray Chest. 3 patients had severe disease requiring Oxygen. Details of symptoms are described in table 1. 8.3% patients required Oxygen, no one required mechanical ventilation and no deaths reported. Out of the 36 patients, 92% were in their third trimester, 5% were in second trimester, 3% were in first trimester. 19 patients had vaginal deliveries, 9 had C-sections and the reasons for C-section and maternal and fetal outcomes are described in table 2. Fetal growth restriction was noted in 2. No fetal deaths reported.
Conclusions: In our study, we found that patients presenting with obstetric complaints or for delivery are more often asymptomatic which suggests a universal protocol to carry out testing for women admitted to the hospital. Inspite of being at the epicenter, we did not see any adverse outcomes in our patients who were SARs-CoV2 PCR positive during the surge of the pandemic. Very few patients had severe disease who required Oxygen and majority of the symptomatic patients had mild disease. A significant proportion of patients had C-section in our study similar to previous reports from NYC. The reasons for C-section were failed Induction of Labor, severe Fetal Growth restriction and decreased fetal movements, oligohydramnios and breech presentation and preeclampsia with severe features. One patient in her second trimester who required Oxygen had decreased fetal movement and fetal tachycardia. More studies are needed to understand if COVID-19 can increase the proportion of operative delivery and certain fetal outcomes. Although the outcomes were promising in our study which has a small sample size, until we have more evidence, we need to be concerned regarding the maternal and fetal outcomes in SARs-CoV2 PCR positive pregnant women. Long term effects of the virus on the mother and baby needs to be explored. To prevent maternal and fetal mortality and morbidity, universal screening for all pregnant women admitted to the hospital should be in place.