Case Presentation: After suffering a left-sided middle cerebral artery stroke and subsequent right sided weakness, an 85-year-old female fell and sustained a fracture of her right intertrochanteric femur. She initially had an ORIF at an outside hospital, but this subsequently failed and the patient had continued pain. She had repeat x-ray imaging of her femur one month later, which demonstrated erosion and migration of the nail through the femur.
At our facility, this patient was then evaluated for a revision and repair of her ORIF by orthopedic surgery. She underwent a total hip arthroplasty with ORIF of her greater trochanteric fracture. In the following month during her rehabilitation, she had an episode of bronchitis which was treated with azithromycin and a urinary tract infection (UTI) which was treated with levofloxacin and cephalexin.
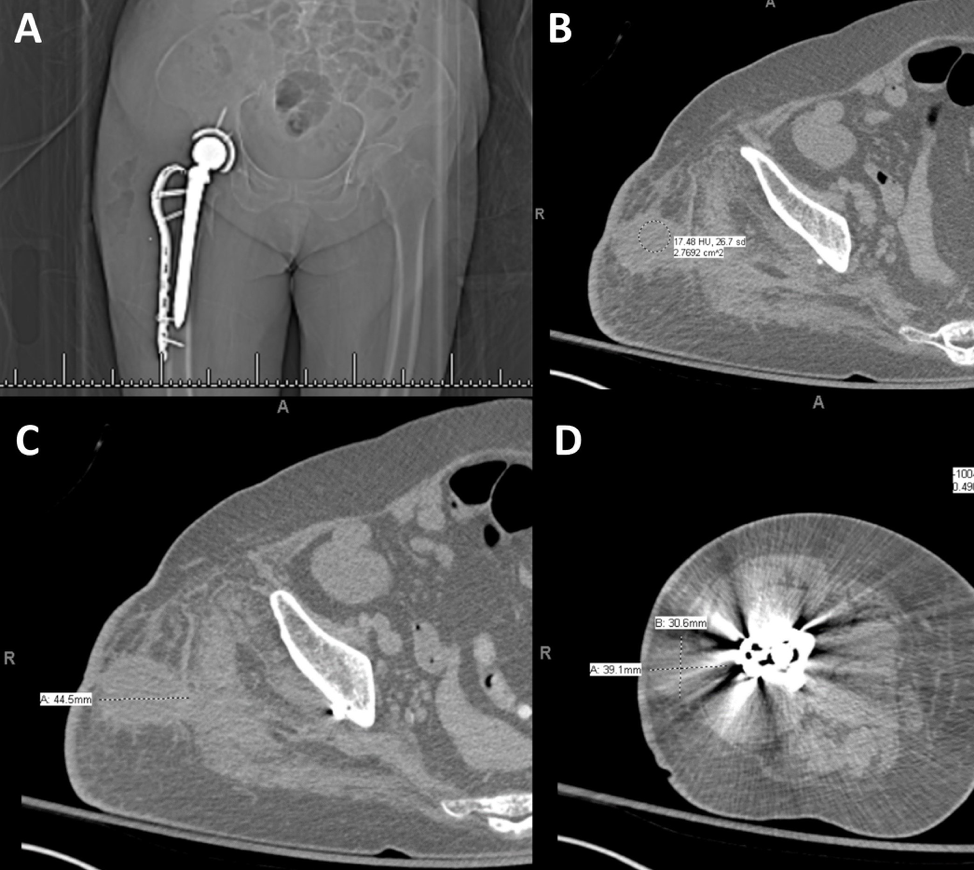
One month after discharge from her total hip arthroplasty and revision, she was seen by orthopedics outpatient and was noted to have increasing right hip pain, in addition to erythema and serosanguinous drainage at the incision site. She was started on cephalexin for a presumed infection. Two days later, her hip pain significantly increased and she sought care at an emergency department for re-evaluation. A CT of the lower extremity without contrast was performed and showed a large, gas-containing collection in the lateral soft tissues of the right pelvis/femur, extending from the iliac crest through the proximal femur, involving the right gluteal musculature— concerning for infection. The patient was taken to the operating room the next day where necrotic and purulent material was found and surgically debrided. Cultures obtained were consistently positive for Clostridium difficile (C. diff), which was treated with piperacillin/tazobactam and metronidazole for six weeks. Cultures were found to be susceptible to amoxicillin/clavulanate and thus following the patient’s six week course of piperacillin/tazobactam and metronidazole, her regimen was changed to amoxicillin/clavulanate for indefinite suppression.
Discussion: Classically, C. diff has a predilection for the colon and causes pseudomembranous colitis. Here, we present the first case of a C. diff infection of the hip in an immunocompetent patient without involvement of the colon. Increased clinical suspicion is warranted in immunocompromised patients, such as those with diabetes mellitus, HIV, or patients on chronic immunosuppressive drugs such as high-dose steroids and immunomodulators. However as evidenced in this case, immunocompetent patients may be equally susceptible.
It is interesting to note that the infection responded to the antibiotics that are frequently the culprit of causing the more prevalent colonic C. diff infection. In this case, the patient was effectively treated with piperacillin/tazobactam and metronidazole for six weeks and was culture free at 6-week follow up with suppression with amoxicillin/clavulanate.
Conclusions: We present the case of an 85-year-old female with a C. diff infection of the hip in the absence of colonic involvement. This is an extremely unusual presentation as this is the first known case of C. diff within the hip of an immunocompetent patient. It is quite significant that the infection and toxins were able to cause injury to the musculoskeletal tissue, when it is usually known to cause disease in the colonic mucosa. Further studies on therapeutic regimen and follow up periods need to be performed to elucidate the optimal strategies for successful treatment of these patients.