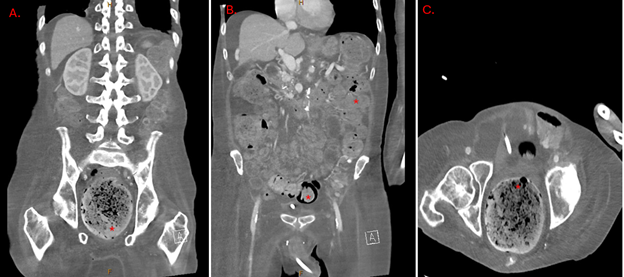
Case Presentation: Stercoral colitis (SC) is an uncommon yet life-threatening inflammatory condition caused by fecal impaction in the colon, leading to increased intraluminal pressure, ischemia, and inflammation. If untreated, complications such as necrosis, perforation, and sepsis can result in mortality rates as high as 63%. Clostridium species, particularly C. perfringens and C. ramosum, are rare causes of bacteremia but are associated with significant mortality. This report details a unique case of dual bacteremia with C. perfringens and C. ramosum in a patient with SC. A 60-year-old male with chronic obstructive pulmonary disease, type 2 diabetes, hypertension, and cachexia presented from his nursing home with hypotension, altered mental status, and shortness of breath. On arrival, his oxygen saturation was below 88% on room air despite baseline use of 1-2 liters of nasal oxygen. Examination revealed a cachectic, lethargic patient with generalized abdominal tenderness, distension, diminished bowel sounds, and confusion. Vital signs included blood pressure of 70/60 mmHg, respiratory rate of 27 breaths per minute, and a temperature of 36.7°C. Laboratory findings showed a white blood cell count of 5200/µL with 14% bandemia, platelets at 114×10³/µL, and an elevated lactate of 4.35 mmol/L. Imaging revealed a right lower lung infiltrate, fecal impaction, and findings consistent with stercoral colitis on CT. Initial treatment included antibiotics, bowel disimpaction, and supportive care. Blood cultures later identified C. perfringens and C. ramosum, prompting escalation to high-dose penicillin G and clindamycin. Despite aggressive resuscitation, the patient developed refractory hypotension and passed away on the third hospital day.
Discussion: C. perfringens and C. ramosum bacteremia, though rare, can lead to rapid clinical deterioration, particularly in patients with underlying conditions such as diabetes, immobility, and SC. SC, an inflammatory condition resulting from chronic fecal impaction, is associated with ischemia and potential perforation, contributing to systemic infections. Diagnosis relies on high clinical suspicion and imaging, while treatment requires prompt antibiotics and, in severe cases, surgical intervention. The combination of C. perfringens’ toxin-mediated erythrocyte destruction and the polymicrobial nature of the infection likely contributed to the poor outcome.
Conclusions: This case underscores the need for early recognition and aggressive management of stercoral colitis and associated Clostridium bacteremia, particularly in vulnerable populations. To our knowledge, this is the first reported case of co-infection with C. ramosum and C. perfringens in a patient with SC. Early diagnosis and a multidisciplinary approach are critical to improving outcomes in such high-risk scenarios.