Background:
Acute upper GI bleed (UGIB) is a major cause of hospital admissions, with peptic ulcers being the most common cause. In addition to pre-endoscopic PPI and urgent endoscopic intervention, current consensus guidelines recommend intensive continuous PPI infusion for 72hrs to decrease the risk of re-bleeding in patients with high risk features. However, a recent systematic review and meta-analysis demonstrated intermittent intravenous PPI therapy to be non-inferior to continuous therapy in these patients. A cost minimization analysis was conducted to compare cost outcomes and determine the uncertainty around these costs. We also determined the difference in re-bleeding probabilities required to make the intensive continuous PPI infusion the lower cost strategy.
Methods:
A cost minimization model designed from an institutional perspective was used to estimate our cost outcomes. The intensive continuous PPI infusion strategy was modeled on the International Consensus Upper Gastrointestinal Bleeding Conference Group 2010 recommendations; the intermittent dosing strategy, from the systematic review and meta-analysis (Sachar et al., JAMA Intern Med 2014). A probabilistic sensitivity analysis (Monte-Carlo Simulation) was used to determine the uncertainty around these costs given each strategies’ re-bleeding probability estimates (beta distributions). A sensitivity analysis on re-bleeding probability was performed to determine the probability difference required to change the preferred strategy. Parameters for nursing and pharmacy costs were derived from internal operational values. Drug costs (Pantoprazole) were acquired using both internal drug cost and average wholesale price (AWP) (Lexicomp). The average cost for treating an UGIB (ICD-9: 532, 533, 534) was estimated from our EDW (Enterprise Data Warehouse) and the HCUP National Inpatient Sample 2012.
Results:
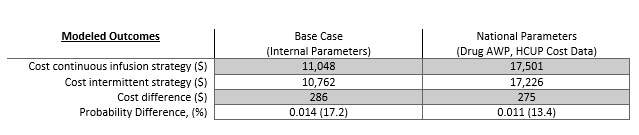
The models comparing internal and national parameters yielded similar results, with the intermittent strategy resulting in slightly lower cost. The probabilistic sensitivity analysis (1000 trials) yielded no trials where the continuous infusion strategy was less costly than the intermittent dosing strategy for either set of parameters. The probability difference required to change the preferred strategy was around 0.01 for both sets of parameters.
Conclusions:
From an institutional perspective use of an intermittent PPI strategy yields modest cost savings. However with an estimated 71,000 UGIB hospitalizations (HCUPS 2012 data) occurring a year, switching to an intermittent PPI strategy could save the nation nearly $19.8 million. As a result, if the non-inferiority finding proves to be durable, consensus guideline groups should consider reviewing current guidelines to favor intermittent PPI treatment in patients with UGIBs.