Case Presentation: Introduction:
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia. In the past decade, catheter ablation of AF has evolved from an investigational procedure to a frequent therapeutic one. Phrenic nerve injury (PNI) is a complication of ablation that internists should be familiar with, due to its increasing incidence.
Case:
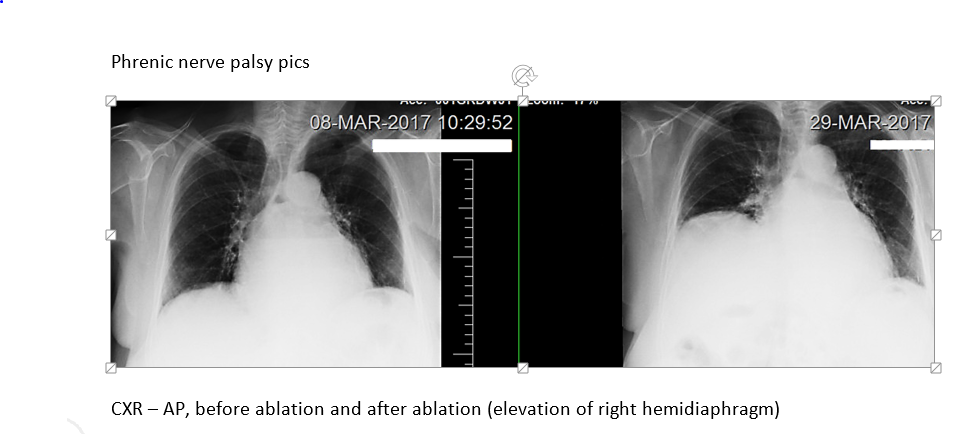
A 77-year-old Caucasian female presented with dyspnea and chest pain for 8 days. One week ago, she had undergone radiofrequency catheter ablation for persistent symptomatic AF. PMH included heart failure with preserved ejection fraction and mild COPD. She led an active lifestyle, did not require oxygen, and had quit smoking 10 years ago. After the ablation, she reported dyspnea even during office visits, which were attributed to heart failure. She had been given increasing doses of diuretics which did not relieve her symptoms. On physical exam, she was in mild distress. Pulse oximetry was 90%. Her weight had not increased and she had no clinical signs of heart failure. Laboratory work up revealed WBC of 10,000, normal electrolytes and negative troponin. ABG showed paO2 of 62 mm Hg and EKG did not reveal signs of ischemia. CXR demonstrated a grossly elevated right diaphragm. Sniff test performed under fluoroscopy showed paradoxical elevation of the right hemidiaphragm with inspiration, compared with rapid descent of the left hemidiaphragm, confirming right hemidiaphragm paralysis. Patient’s dyspnea was proportionate to the degree of physical activity and hence she did not need treatment by surgical plication. She was discharged with home oxygen. She has remarkably improved and her symptoms have resolved.
Discussion: Ectopic discharges from pulmonary veins have been discovered to be an important cause of atrial fibrillation which can be treated by ablation. Phrenic nerve injury is an important complication of this therapy due to the close anatomic relationship of the phrenic nerve to the heart. In our patient, the right phrenic nerve, which runs along the lateral surfaces of the superior vena cava and right atrium, was injured by energy delivered to the adjacent area during ablation. The phrenic nerve is more sensitive to heat because its myelin sheath retains the heat, although PNI has also been reported after cryoablation.
When clinically suspected, PNI and unilateral diaphragmatic paralysis can be diagnosed by the absence of normal downward movement on quiet and deep breathing, with paradoxical upward motion on sniffing (Sniff Test). Fortunately, the condition is often asymptomatic with good prognosis.
Conclusions: In conclusion, internists will greatly benefit in familiarizing themselves with this condition as more and more of our patients are diagnosed with AF and undergo ablation. It is important to develop the clinical suspicion and to also correlate onset of symptoms to the ablation, since the symptoms can mimic that of comorbid conditions (CHF,COPD). This can lead to missed or delayed diagnosis.