Background: The number of individuals with dementia in the U.S., currently estimated at 5.3 million, is projected to triple by 2050. For patients with cognitive impairment, the unfamiliar and stressful hospital environment often requires constant observation (CO) to ensure patient safety. The use of constant observation (CO) in the hospital setting, while originating in patients with psychiatric disorders at risk for self-harm, is increasingly being used to solve other clinical challenges. Our study aimed to assess hospital providers’ perceptions and practices with regard to the use of CO for hospitalized older adults with cognitive impairment.
Methods: We conducted an IRB-approved, multi-center, cross sectional, anonymous survey with registered nurses (RNs), nurse practitioners (NPs), and physicians (MDs) in a large, metropolitan area. Survey items were evaluated by a multidisciplinary panel of experts including geriatricians, hospitalists, biostatisticians and researchers.
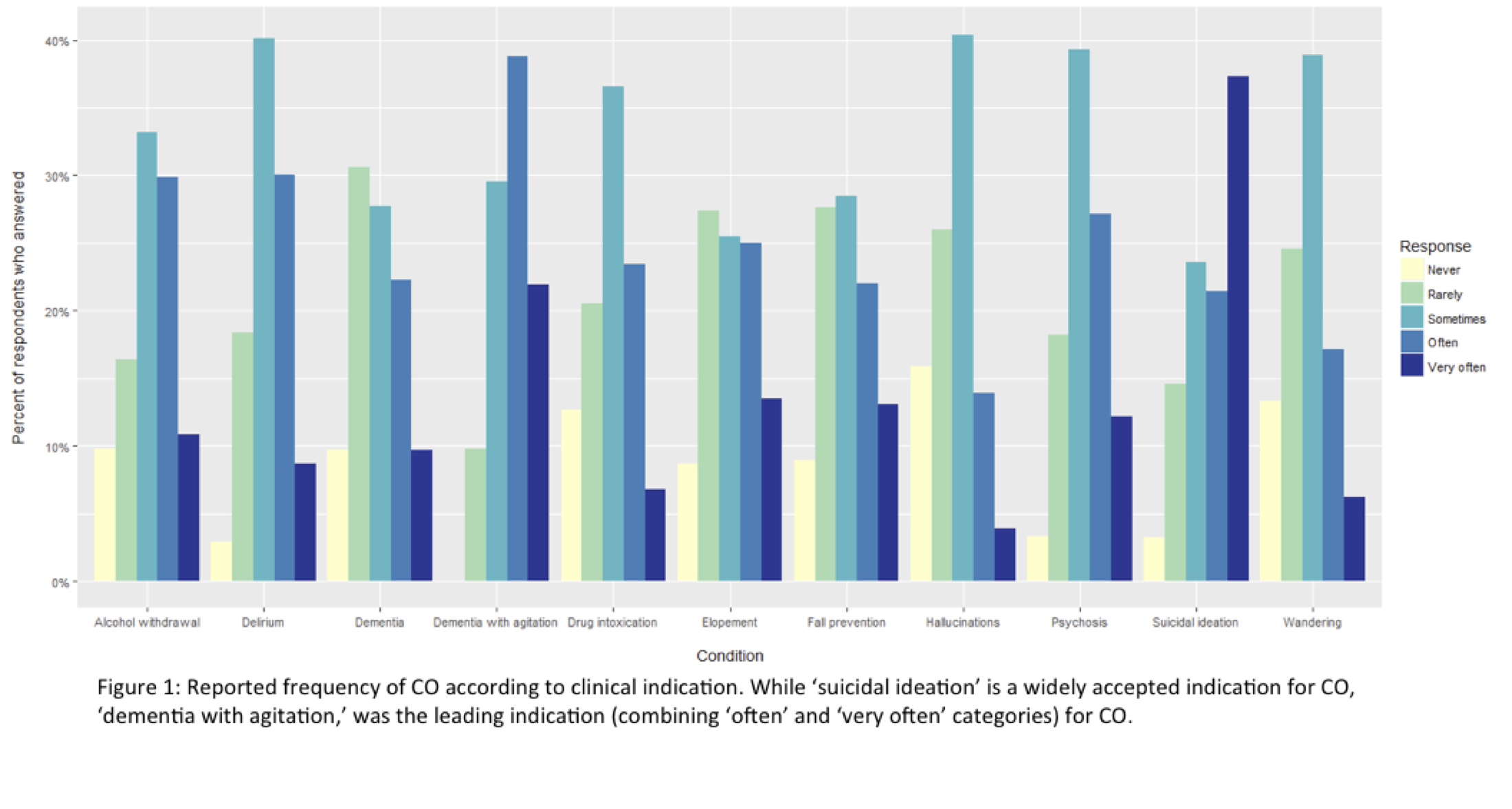
Results: Of the 543 surveys distributed, 231 were completed (42.5% response rate). Nurses constituted the largest group of participants (49.07%), followed by physicians (35.65%), and most were female (75.6%). 44.8% were White, 25.9% were Asian, and 14.2% were Black. Most respondents worked on medical units (67.5%), and 84% reported at least 1 patient per week requiring CO, while 24.4% reported at least 2 CO cases per week. Most frequent indications for CO (Figure 1) were dementia with agitation (60.7%) and suicidal ideation (58.7%); and 77.2% reported most frequent CO use was in patients over 60 years old, while 62.3% reported most frequent CO use in patients over 70. Most (59.9%) continued CO at least ‘over a few days’. CO was most commonly performed by a nurse assistant (93.9%). While 76% of participants felt that CO was beneficial for patient care, almost half (47.3%) reported that they felt pressured to decrease CO use. Most commonly reported methods for decreasing CO use were: enhanced supervision (92.6%), family members (36.1%), and cohorting (33.2%). Most participants (77.9%) perceived those who perform CO to lack training, and 51.4% felt that more resources are required to improve CO in the hospital.
Conclusions: Our study highlights the widespread use of CO for hospitalized patients with dementia who display behavioral disturbances. Given the high cost of CO as well as the lack of national guidelines, there is an urgent need to develop cost-effective, sustainable models that ensure quality care, dignity and respect for this vulnerable population and their caregivers.