Background: Improving the appropriate use of peripherally inserted central catheters (PICC) has been shown to reduce the rates of PICC-associated complications. However, quality improvement (QI) programs that promote appropriate PICC use may require significant financial investment. We evaluated the cost-effectiveness of the Michigan Hospital Medicine Safety (HMS) PICC QI initiative, a physician-led, performance-incentivized, QI intervention to improve appropriate PICC use at hospitals participating in a state-wide multi-institutional collaborative funded by Blue Cross Blue Shield of Michigan and Blue Care Network (BCBSM/BCN).
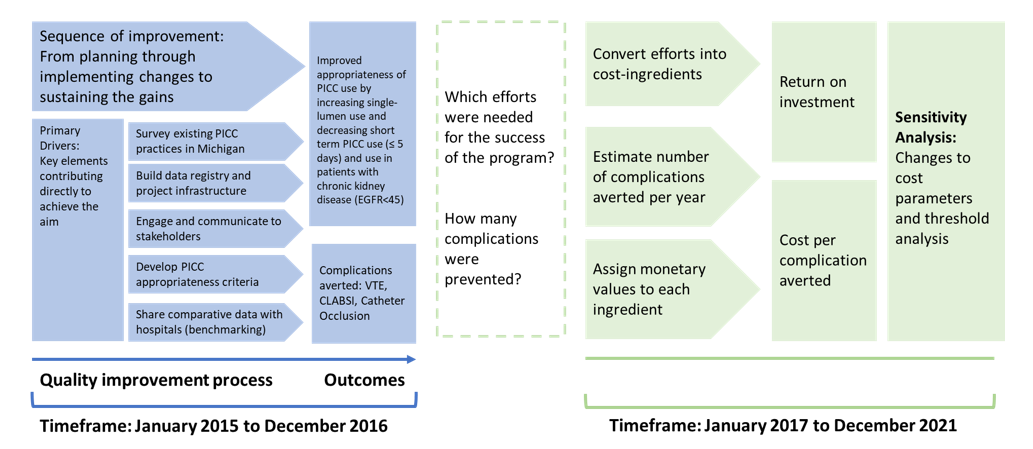
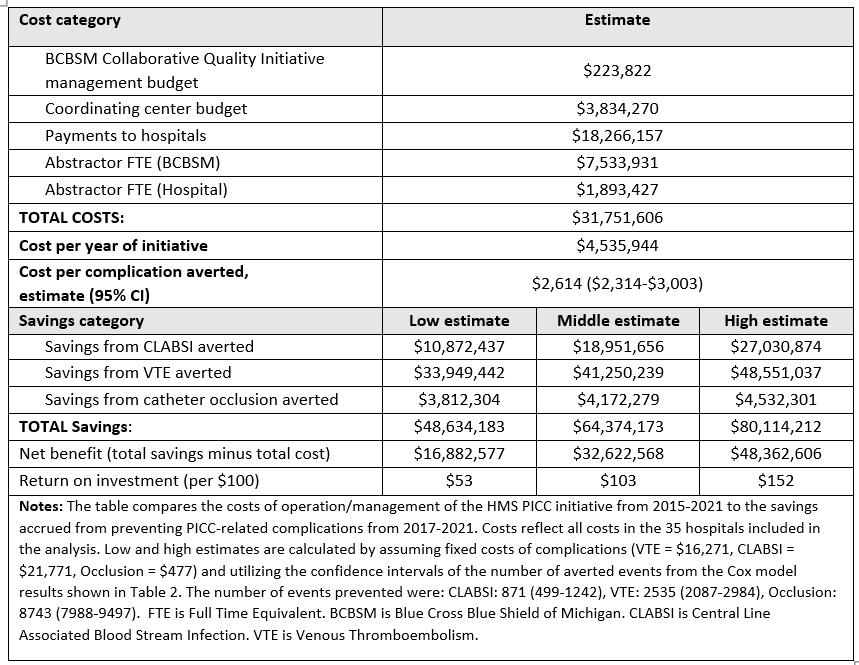
Methods: We assessed the cost-effectiveness of the HMS-PICC QI initiative in 35 hospitals across the 7-year span of the project from Jan. 2015 – Dec. 2021. The pre-intervention phase was from Jan. 2015 – Dec. 2016 and the intervention phase from Jan. 2017 – Dec. 2021. Following evidence-based guidelines, the initiative focused on improving PICC appropriateness by increasing the proportion of single-lumen PICCs placed, decreasing short-term PICC use (≤5 days), and reducing use in patients with advanced chronic kidney disease (CKD), defined as eGFR< 45 ml/min/1.73m2. Improvement strategies included providing benchmarked hospital data, garnering support/guidance from HMS physician champions, and developing a toolkit to guide hospitals through the PICC QI process. Adherence to QI measures were assessed through regular data collection and incentivized through a pay-for-performance scorecard. Costs for implementing and sustaining the QI intervention were assessed using recognized frameworks for economic evaluations1. Implementation costs included payments to data abstractors, QI staff salaries, incentive payments to hospitals, costs for hosting quarterly meetings, and costs related to hospital site-visits and audits2. Effectiveness was calculated from propensity score matched observations across the pre-intervention and intervention time periods for complications (i.e., venous thromboembolism [VTE], central line-associated blood stream infection [CLABSI], and catheter occlusion). Cost-effectiveness was presented as incremental cost-effectiveness ratios including costs per averted complication during the 60-month intervention period.
Results: There were 17,418 PICCs placed in the pre-intervention period and 26,004 PICCs in the intervention period. When comparing pre-intervention to intervention period, single-lumen PICC use increased (38.7% vs 59.3%, p< 0.1), short-term PICCs decreased (29.9% vs. 15.0%, P<.01), and the use of PICCs in patients with CKD was reduced (32.0% vs. 23.3%, P<.01). The estimated number of PICC complications prevented during the post-intervention period included 871 CLABSIs, 2,535 VTE events, and 8,743 catheter occlusions. The total cost for implementing the QI project was $31.8 million. The total cost-offset related to avoiding the cost of complications was $64.4 million. The savings per complication averted was $2,614 (95% CI: $2,314-$3,003) and the return on investment was $103 per each $100 invested.
Conclusions: We found that a large-scale, multi-hospital QI initiative to improve appropriate PICC use can be implemented and sustained with cost-effectiveness over long observation periods. These results may provide evidence to policymakers who wish to implement similar QI initiatives.