Background: Coronavirus-19 (COVID-19), primarily a respiratory virus, can affect multiple organs, including the heart. Cardiac complications can affect 20-30% of COVID-19 patients and lead to worse morbidity and mortality. Cardiovascular complications can include myocarditis, acute myocardial infarction, heart failure, and arrhythmias Myocarditis is a well-known complication among COVID-19 infections, with limited large-scale studies evaluating outcomes associated with COVID-19-related Myocarditis.
Methods: We used the National Inpatient Sample (NIS) database to compare COVID-19 patients with and without Myocarditis. A total of 1,659,040 patients were included in the study: COVID-19 with Myocarditis (n = 6,455, 0.4%) and COVID-19 without Myocarditis (n = 1,652,585, 99.6%). The primary outcome was in-hospital mortality. Secondary outcomes included mechanical ventilation, vasopressor use, sudden cardiac arrest, cardiogenic shock, acute kidney injury requiring hemodialysis, length of stay, health care utilization costs, and disposition. We conducted a secondary analysis with propensity matching to confirm results obtained by traditional multivariate analysis.
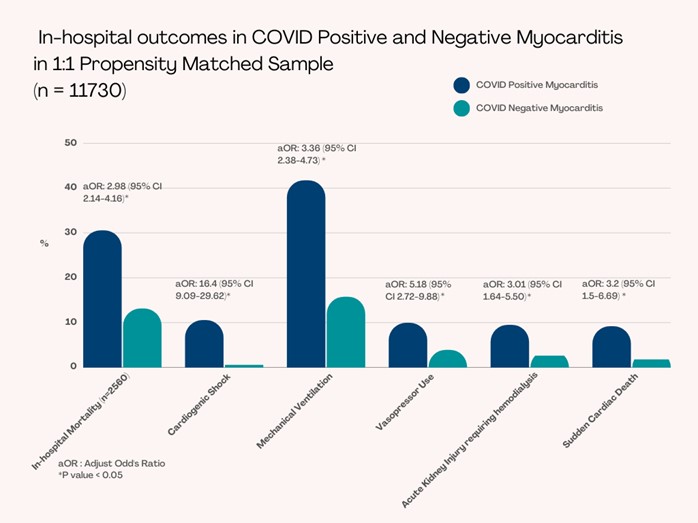
Results: COVID-19 patients with myocarditis had significantly higher in-hospital mortality compared to COVID-19 patients without Myocarditis (30.5% vs. 13.1%, adjusted OR: 3 [95% CI 2.1-4.2], p < 0.001). Mortality in COVID-19 patients with myocarditis was significantly higher among younger patients: years ≥ 18-29 (1.5% vs. 0.6%, p < 0.001), years 30-49 (7.3% vs. 4.9%, p < 0.001, years 50-69 (39.1% vs. 30.4%, p < 0.001) as compared to COVID-19 patients without myocarditis. Patients over the age of 50 had a significantly increased risk of mortality (age 50-69, aOR: 4.4 [95% CI 1.6-12.2], p = 0.005; age ≥ 70, aOR: 5.5 [95% CI 1.8-16.5], p = 0.002). Higher mortality was observed in patients requiring mechanical ventilation (aOR: 6.1 [95% CI 4.1-9.1], p < 0.001), vasopressor use (aOR: 1.8 [95% CI 1.0-3.0], p = 0.03), and developing AKI (aOR: 1.7 [95% CI 1.2-2.6], p = 0.004). Underlying cardiovascular comorbidities were not statistically significant predictors of mortality.Patients who presented with COVID-19 with myocarditis required more mechanical ventilation (41.7% vs. 15.8%, aOR: 3.4 [95% CI 2.4-4.7], p < 0.001), higher vasopressors use (9.9% vs. 3.9%, aOR: 5.2 [95% 2.7-9.9], p < 0.001), and experienced more cardiogenic shock (10.5% vs. 0.6%, aOR: 16 [95% CI 9.1-29.6], p < 0.001); however, did not require significant mechanical circulatory support (2.6% vs. 0.5%, aOR: 2.5 [95% CI 0.5-11.4], p = 0.29). These patients also had statistically significant higher rates of acute kidney injury requiring hemodialysis (9.5% vs. 2.6%, aOR: 3.0 [95% CI 1.6-5.5], p < 0.001) sudden cardiac arrest (9.1% vs. 1.8%, aOR: 3.2 [95% CI 1.5-6.7], p = 0.002) and higher overall hospitalization cost.
Conclusions: Our study found that myocarditis in COVID-19 patients was associated with worse outcomes both in terms of morbidity and mortality, including increased acute kidney injury needing hemodialysis, cardiogenic shock with vasopressor support, mechanical ventilation and sudden cardiac death. Vaccination may play a pivotal role in reducing the incidence of COVID-19-related myocarditis. Increased risk of worse outcomes coupled with limited treatment options highlights the need for further research for effective vaccination and treatment strategies to improve outcomes in COVID-19-positive patients.