Background: The SARS-CoV-2 outbreak presents an infection control challenge to deliver care in a safe environment for patients and healthcare workers (HCW), further complicated by uncertainty regarding the nature of contagion of SARS-CoV-2 and PPE supply chain. On March 15, 2020, we introduced “medical distancing” rounding guidelines, with the aim of reducing transmission of COVID-19 when PPE supply and testing capability was limited. Specific recommendations included: maintaining > 6 feet distancing from peers, reducing the number of patient visits if non-urgent, utilizing telephone or virtual modes of communication with patients, and limiting the number of bedside rounding providers.
Methods: We performed a qualitative study of our hospitalists to characterize how medical distancing measures impacted perceptions around the quality of care delivered. An anonymous 11 item questionnaire was designed to capture hospitalist perspectives on 5 domains of care: timeliness, communication, diagnostic accuracy, efficiency and emotional connection (rated on a 3-point scale: negative, neutral, positive). From 5/9/2020 to 6/1/2020, the survey was administered to 57 UCSD hospitalists via REDCap. Demographic information and survey responses were reported as frequencies. SPSS was used for statistical analysis. Responses were binned/dichotomized for the sake of statistical testing. For comparison testing, either Chi-squared or Fisher’s exact testing were used; 2-sided p-values are reported.
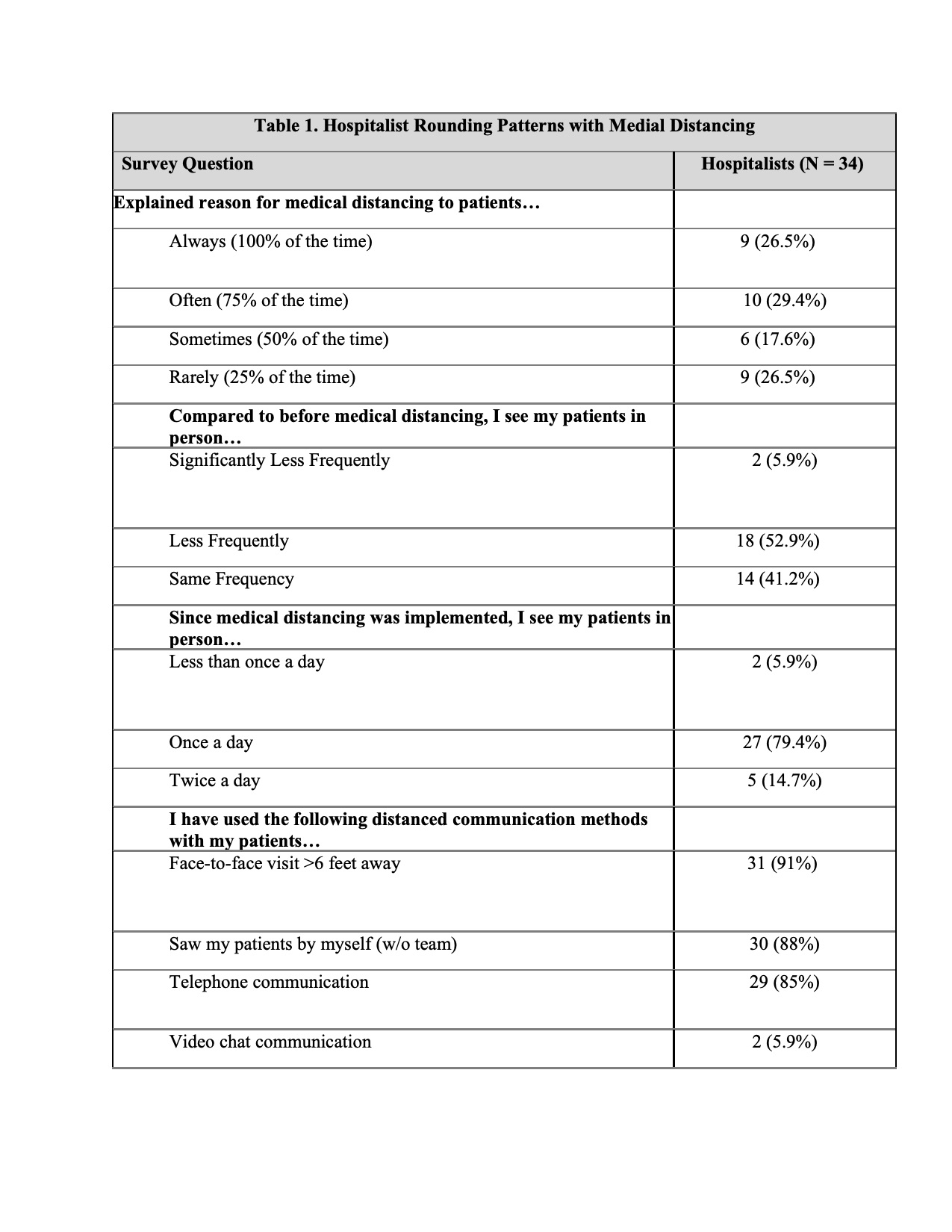
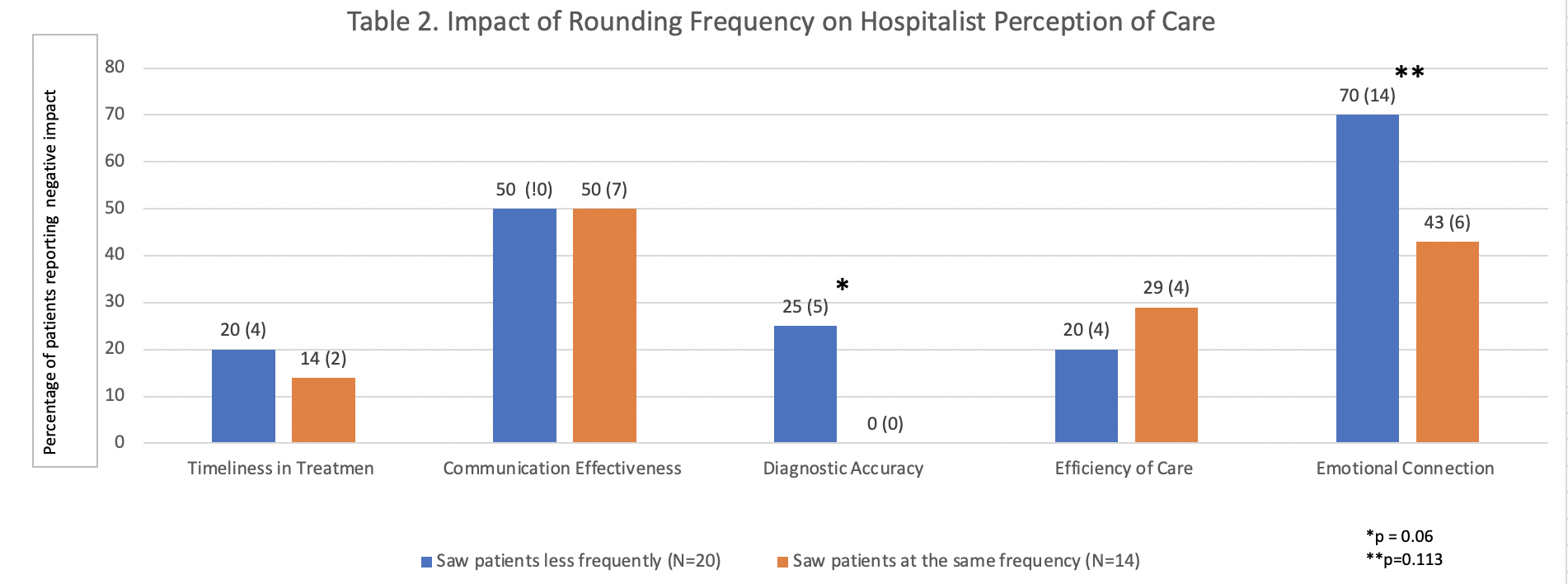
Results: The survey was completed by 59.6% (N=34) of hospitalists. Average length of hospitalist employment reported was ≥ 5 years, with majority of respondents being daytime hospitalists. The majority of hospitalists had cared for less than 10 patients with COVID-19 at the time this survey was conducted (56%). When compared to pre-COVID, 52.9% of hospitalists reported seeing patients in-person less frequently. Most hospitalists saw patients at least once per day (79.4%), with 5.9% seeing patients on average less than once per day. Comparison of hospitalists who reported seeing patients less frequently to those who did not showed no statistically significant difference in the domains of timeliness in treatment, communication effectiveness, and efficiency of care. Near significant differences were seen in diagnostic accuracy and emotional connection, where 25% of hospitalists who saw patients less frequently reported an impact of medical distancing on diagnostic accuracy, compared to 0% who saw patients with the same frequency (p=0.06). 70% of hospitalists who saw patients less frequently reported a negative impact of medical distancing on emotional connection, compared to 43% who saw patients with the same frequency (p=0.11) (Table 2).
Conclusions: We saw no difference in perceived timeliness, communication effectiveness and efficiency amongst hospitalists who decreased visitation frequency compared to those who didn’t. The results of this study also show that physicians perceive the most significant impact of medical distancing to be on the emotional connection with patients and diagnostic accuracy. Inpatient based distant care models achieved through decreased frequency of in person visitation are a potential way to conserve PPE, decrease transmission risk and maximize personnel in resource limited settings. Further studies are needed to assess if video platforms and enhanced remote monitoring can close the gap of decreased emotional connection and care quality from the physician viewpoint.