Background: The SARS-CoV-2 (COVID-19) pandemic has led to challenging staffing situations for health systems. Rapid increases in patient volumes, coupled with clinician illness, need for quarantine/isolation as well as other workforce restrictions, have required systems to become nimble in clinician staffing. To overcome these challenges, novel approaches have been utilized including the employment of non-traditional clinician workforces (e.g. Orthopedics-trained clinicians) to provide inpatient care traditionally provided by hospitalists. These multi-departmental efforts require careful execution given the number of individual clinicians involved.
Purpose: In response to projected increases in COVID-19 censuses at the University of New Mexico Hospital (UNMH) during the first wave of the pandemic, a COVID-19 Floor Incident Command Staffing Team (CICST) was created to guide COVID-19 surge staffing deployments.
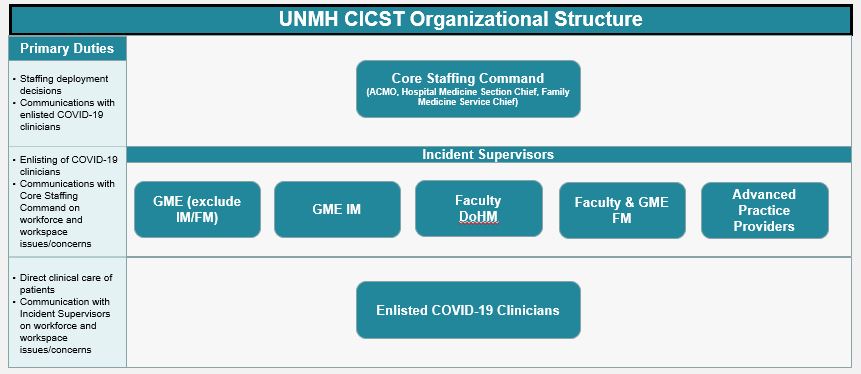
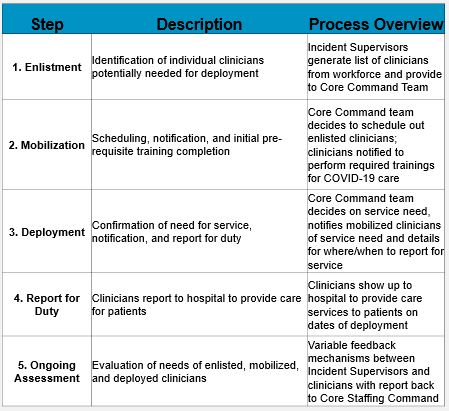
Description: The CICST consisted of a Core Staffing Command group – involving the hospital associate chief medical officer and Hospital Medicine and Family Medicine inpatient service directors – as well as Incident Supervisors who provided a direct line of communication to enlisted workforces (Figure). CICST members jointly created a charter which included consistent nomenclature and process of staffing decisions. Deployment steps loosely followed processes established by U.S. military forces (Table).Through the peak of the first wave, CICST core members met thrice weekly to review staffing. Meetings were structured for effective decision making and consisted of 1) review of hospital census; 2) review of available projections; and 3) vote on staffing decisions. Opportunity to discuss feedback from Incident Supervisors on workforce needs was also provided. Within deployments, hospitalists were deployed first followed by non-hospitalist clinicians.The CICST also led system-wide communications related to deployments. Dashboards were created to provide scheduled clinicians with situational awareness. Communications were specifically worded to acknowledge uncertainty and openness of process as well as to provide additional avenues for support.A total of 224 clinicians across UNMH were enlisted in surge scheduling. By May 5, 2020, floor COVID-19 service censuses peaked at 44 patients by which time five separate COVID-19 teams had been deployed. 52 of the 224 enlisted clinicians were ultimately deployed.
Conclusions: The CICST enabled an organized way to enlist and deploy a novel workforce to provide inpatient COVID-19 care. Through a shared decision-making model involving key stakeholders in design and implementation, CICST was able to nimbly make challenging staffing decisions involving clinicians at a large academic medical center.