Background: Croup affects more than 1.4 million children under the age of six in the United States annually. Up to 6% of children with croup are hospitalized at an estimated annual cost of $56 million. Guidelines for Emergency Department (ED) and inpatient management of croup vary and generally rely on limited evidence. Specifically, admission and discharge criteria are often institution-specific and formed by group consensus. As a result, ED and inpatient croup management and outcomes vary significantly. Additionally, most children admitted with croup do not receive further medical intervention after admission from the ED.
Purpose: At our institution, we found variation in admission and discharge decision making in patients with croup, inspiring the creation of care guidelines to address provider uncertainty and promote standardization. For the ED, we developed admission criteria with the aim of reducing the proportion of patients that did not receive medical intervention after admission. For admitted patients, we standardized discharge criteria with the aim of reducing the mean and standard deviation of length of stay.
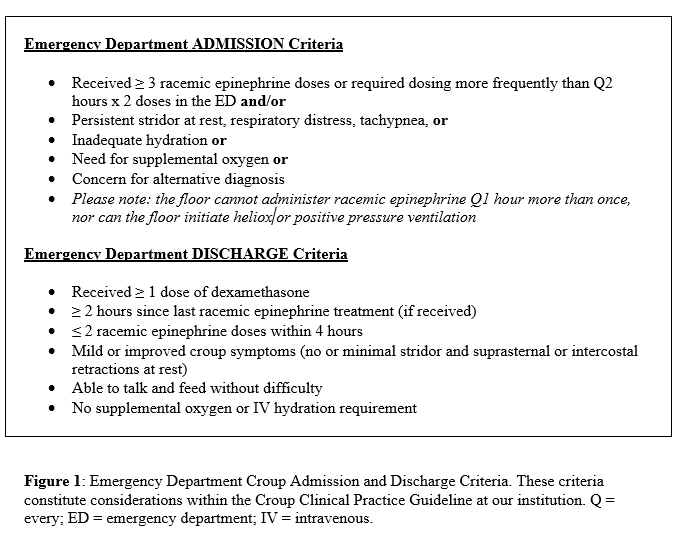
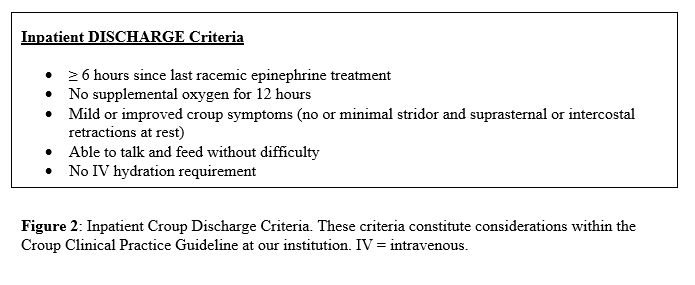
Description: We formed a multidisciplinary team of pediatric hospitalists, ED physicians and nurse practitioners, registered nurses, respiratory therapists, pharmacists, and quality improvement consultants. We began with a review of peer guidelines, then completed a literature review and evaluation using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria. We completed an external benchmark with 15 peer institutions using the Pediatric Health Information System (PHIS) database and internal data analysis of patients with croup between 2016 and 2019 to identify specific areas of improvement. We completed department-specific process maps and barrier assessments with stakeholders from the ED and acute care floor and found that admission and discharge criteria varied because of individual provider uncertainty. 2385 patients met our cohort criteria. Our admission rate was 13%, placing us in the top quartile of the benchmarked hospitals. 69% of admitted patients did not receive further medical intervention with nebulized racemic epinephrine (RE) after admission. The mean time between the last dose of RE and discharge was 17 hours with a standard deviation of 10 hours, higher than peer recommendations which range from six to eight hours. We utilized our multidisciplinary panel to form consensus recommendations that focused on reducing variation in LOS and the proportion of patients that did not receive RE after admission. We then created care algorithms for the ED and acute care floor, order sets, and note templates. The two algorithms emphasized the aims defined as most relevant to the delivery of care in the ED and on the acute care floor. See Figures 1 and 2 for admission and discharge criteria.
Conclusions: For institutions seeking to build clinical pathways, we found that the following attributes were key to our success. We were able to increase stakeholder buy-in and create institutionally relevant metrics and goals through external benchmarking and internal data review. The exploration of the literature and our current practices, and comparison to peers, allowed us to focus our improvement efforts and create guidelines that were relevant to and supportive of providers at our institution.