Background: Hospital Medicine (HM) based procedure services have demonstrated improved outcomes for patients by reducing time to procedure, improving throughput, and decreasing length of stay. Notable barriers to service implementation and sustainability include staffing shortages, training, and payment models. Provision of bedside procedural care in the community teaching hospital setting may facilitate access to other Interventional Radiology (IR) based procedures.
Purpose: This community teaching hospital based innovation utilized our long-standing HM Fellowship program to create the procedure service, and embedded highly desired procedural training among residents and fellows to provide ongoing education. The creation of this service was supported by the IR team who in turn was able to increase needed capacity to perform IR specific services.
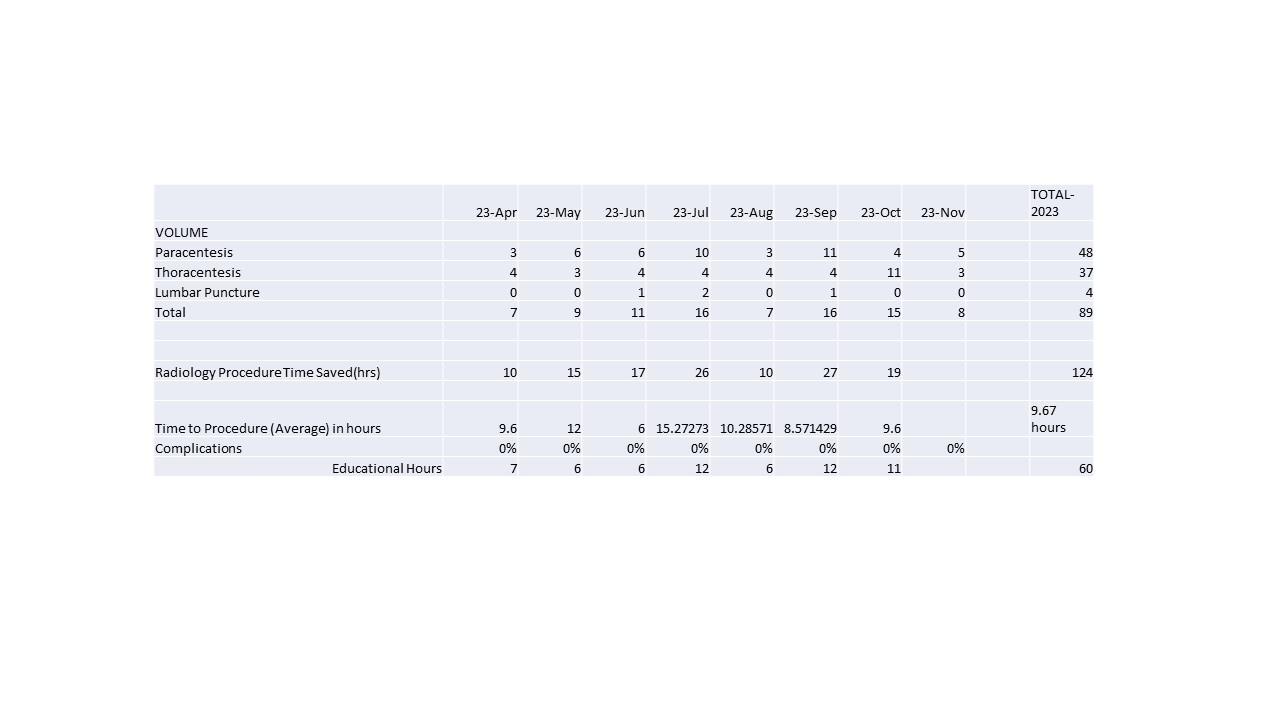
Description: We first assessed demand, and reviewed procedures performed by other subspecialties including IR and critical care medicine. Based on volume and procedure type, as well as high unmet demand for IR services, the HM based procedure service targeted thoracentesis, paracentesis, and lumbar puncture.A hospitalist procedure cart was obtained, with all materials necessary for the bedside procedures. A schedule was created where a proceduralist would be present for a 6 hour period at the beginning of the week. This allowed for patient capture to be obtained over the weekend. Physicians who were privileged would also provide limited services during usual hospitalist shifts.A collaborative effort was initiated with IR to provide mentorship for HM Fellows to gain proficiency and meet numbers for privileges. These now privileged team members anchor the training of current and subsequent fellows, residents and other Hospitalists who are highly engaged in the opportunity to gain these skills. Increasingly procedures on the service are performed with a trainee, readily providing the numbers and experience needed for privileges and team growth. Data was collected over 8 months (figure 1) for the following variables: volume per type of procedure and total (89), time from consult to procedure (avg 9.67 hours), estimated IR time saved (124 hrs.), complication rate (0%), and learner involvement (60 hrs.). In addition to improving above outcomes over time, additional data will be analyzed examining length of stay, throughput, and impact on patient experience. We are also looking at the organizational financial impact and are pursuing a process and business plan to offer procedural services to family medicine residency outpatients- both creating an additional educational opportunity, and providing much needed access to care. Finally we will further assess the impact of offering these bedside services in the critical access hospital setting.
Conclusions: A fellowship based HM procedure service in a community teaching hospital has supported increased access to select bedside procedures as well as other IR services, has markedly enhanced training opportunities for fellows and residents and has preliminarily had high quality outcomes and may facilitate additional outpatient and rural access.