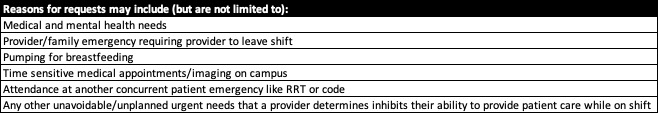
Background: Providers have a variety of situations arise on shift that challenge or inhibit their ability to provide care to patients, sometimes with advanced notice but often without. Most programs have coverage systems in place for emergent needs, but these are less than ideal for immediate and short-term situations (Table 1). Without a set policy, providers are burdened with identifying a colleague to help while at the same time addressing their acute issue causing the need for coverage, putting both patients and providers at risk. Permanent solutions to this issue are difficult given schedules already maximize provider time and budgets for non-revenue generating provider time may not exist.
Purpose: The aim of our intervention was to develop a coverage system to provide immediate, short-term support for any provider until they can return to their duties or a long-term solution is determined, while requiring minimal additional personnel resources.
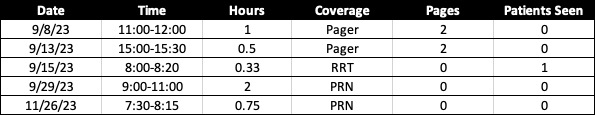
Description: With the support of leadership, a task force was created with stakeholders from scheduling, triage, and parental advocacy, with physician and advanced practice provider (APP) representation. Multiple models were explored, with the goal to provide the most coverage but least strain on the current system. The Emergency Coverage Provider (ECP) was created and the APP admitter, who admits between 7:30 AM and 5:00 PM, was identified for first-line coverage as admitting duties could be paused. A lower acuity service physician functions as backup. The type of coverage requested could be either full transition of care, pager coverage, or as needed (PRN) basis, with the primary provider holding their pager and calling the ECP if a patient needs evaluated at bedside such as during a Rapid Response Team (RRT) activation. Responsibilities are limited to temporary cross coverage and not daily rounding tasks like writing notes or routine orders. Those that use the ECP are not required to disclose the reason for coverage requests but are expected to use judiciously and make good faith effort to minimize impact on teammates and limit transitions of patient care.Policy details were presented at a section meeting and communicated through email, with the pilot starting September 2023. Usage data is collected from ECP providers including coverage time, pages, number of patients seen, and whether this added work caused them to stay past their defined shift end time (Table 2). Data is collected by one member of the task force to preserve anonymity to providers. During the pilot period, ECP usage was higher than initial estimations, totaling 5 times over the first 2 trial months. The ECP was required to pause current duties to provide direct patient care for one rapid response event. Qualitative feedback has been promising, with providers noting the ECP allowed them to handle health issues while returning to shift as well as attend time-sensitive medical appointments rather than call off. After 3 months, formal feedback will be elicited from all providers who have used and served as the ECP.
Conclusions: While the use of the ECP was higher than expected, the burden of actual work absorbed by the position was minimal. Formal feedback is still required, but the initial response to the program has been positive. Further evaluation of the program will determine the impact on the standard back-up program and identify whether this intervention generates a boost in supportive culture within the hospitalist group.