Background: Prolonged intensive care unit (ICU) length of stay (LOS) has been shown to delay patients’ recovery, increase their exposure to the risk of infections, upsurge healthcare costs, and reduce care availability to other critically ill patients. ICU LOS is directly influenced by both medical and institutional factors. The aim of the project is to identify the most common institutional factors causing delays in de-escalations of care within our hospital and implement a directed intervention for improvement.
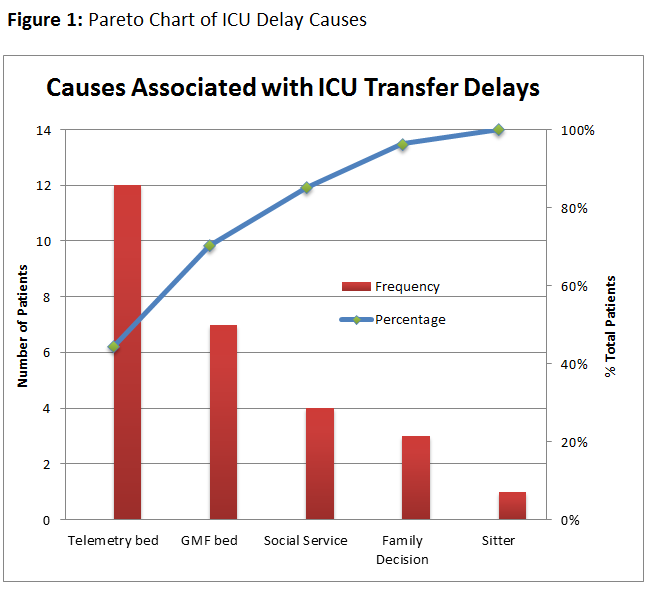
Methods: The project was based in the ICU of an urban community teaching hospital with an average census of 10-14. Baseline data collection of was completed through manual chart review for 4 weeks in December 2017. Prolonged ICU LOS was defined as >12 hours of delay from time patient deemed medically stable for de-escalation in level of care. During baseline data collection, 27 ICU transfer delays occurred. Bed unavailability was the most common reason for delay at 70% (19), with 64% of those delays due to lack of telemetry beds with full details in Figure 1. Based on these findings, an educational intervention based on updated recommendations for telemetry use was created in conjunction with a concurrent project in the Internal Medicine residency program. Residents were given two lectures, one didactic and one case-based to illustrate the updated practice recommendations. Following the intervention, data collection resumed for an additional 4 weeks to evaluate its impact on the lack of telemetry beds associated with ICU transfer delays.
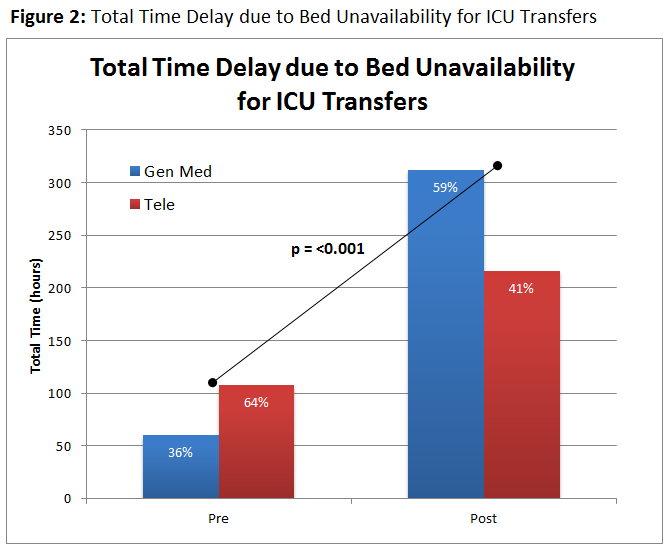
Results: A total of 8 weeks of ICU transfers were reviews, 2 pre-, 6 post-intervention with a total of 43 transfers delays identified. In the pre-intervention period, 5 main categories of institutional factors associated with ICU transfer delays were discovered: bed unavailability (12 telemetry, 7 GMF) – 70%, pending family decisions (4) – 15%, social service needs (3) – 11%, and staffing shortage (1) – 4%. Following the intervention, the proportion of delays due to telemetry bed unavailability decreased from 64% to 41% (p < 0.001), with the daily average delay hours decreasing from 7.2 to 4.8 (p = 0.413). The overall average of 12-hour transfer delays due to bed availability remained stable from 6.5 pre-intervention to 6.7 post-intervention.
Conclusions: Telemetry bed unavailability was a major institutional factor associated with longer ICU LOS. Dedicated provider education on updated telemetry recommendation appeared to reduce total time delay due to lack of telemetry for ICU step-down transfers. However, lack of change in overall ICU transfer delays may relate to other institutional restraints, requiring further evaluation and intervention.