Background: Due to their widespread availability, inflammatory markers are used with increasing frequency, often concurrently, without adding any diagnostic or clinical benefit1,2. While unnecessary labs do not offer any additional benefit, they can be a significant source of physical and emotional distress to patients and their families3-5. In an era that emphasizes high-value, low-cost medical care, providers play an integral role in promoting evidence-based practices to avoid unnecessary laboratory testing. We aimed to decrease the redundant use of inflammatory markers by ≥10% in 12-months.
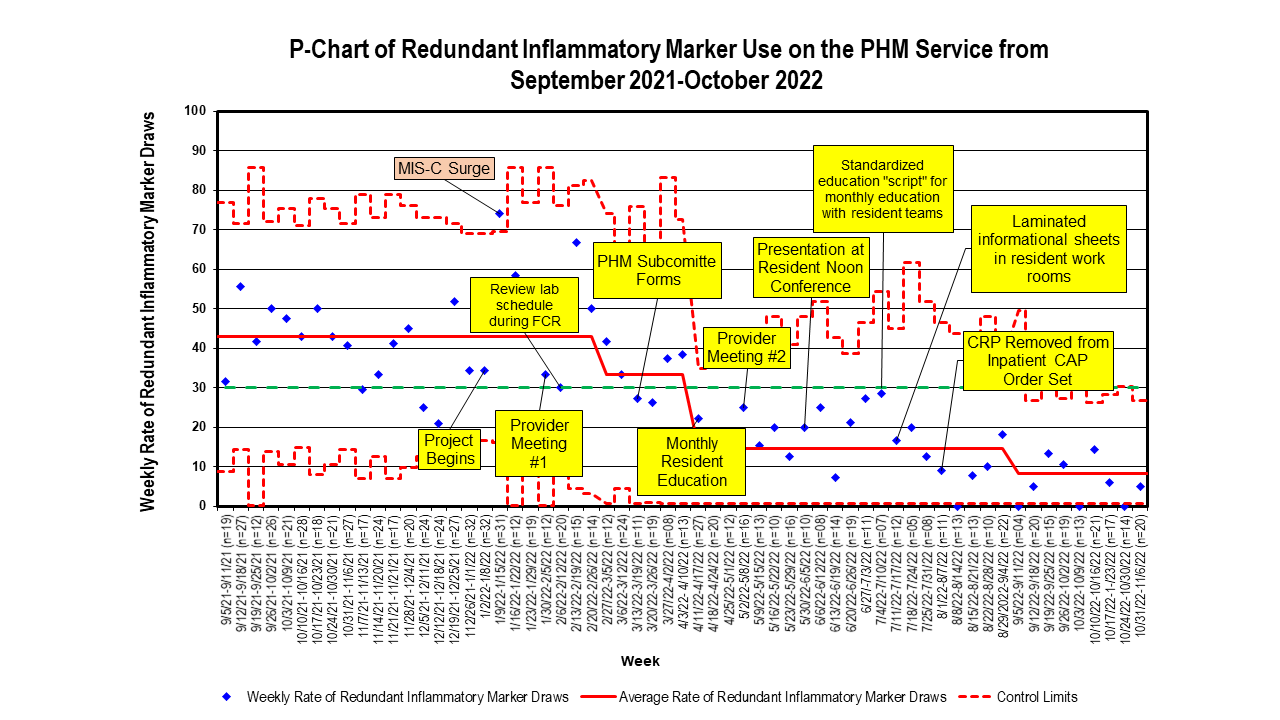
Methods: A quality improvement study was conducted using the IHI Model for Improvement. During the initial phase of project development, there was a division wide presentation detailing project rationale and proposed interventions. Providers were presented with baseline data and the key driver diagram to allow input regarding proposed interventions. Subsequent presentations were given on a quarterly basis. Contents of discussion included pathophysiology of inflammatory markers and review of current evidence-based guidelines with special focus on well-appearing febrile infants, community acquired pneumonia, and sepsis. Institution specific guidelines were also reviewed to highlight the inclusion and/or exclusion of various inflammatory markers. Standardized education scripts were created to guide monthly resident education. Residents were also incorporated through family centered rounds initiatives and laminated reference sheets in team workrooms. Our primary outcome measure was the rate of redundant inflammatory marker use, defined as the use of any two or more inflammatory markers within the same 24-hour period on any given patient. Secondary measures included total inflammatory marker use and number of blood draws. We tracked total number of CBCs as a balancing measure.
Results: From September 2021-December 2021 a total of 821 inflammatory markers were ordered by the PHM service. Approximately half (n=397, 49.1%) of orders were accounted for by 8 out of a total of 27 hospitalists. Inflammatory markers were most frequently obtained for COVID/MIS-C (n=238, 29%) followed by other infections (n=158, 19.2%), non-infectious diagnoses (n=105, 12.8%), sepsis (n=91, 11.1%), viral respiratory illnesses (n = 76, 9.3%), other respiratory diagnoses (n=71, 8.6%), bacterial pneumonia (n=49, 6.0%) and unspecified fever (n=33, 4.0%). The baseline rate of redundant inflammatory marker use was 43%. This was decreased to 8% after 9 months of intervention. The total inflammatory marker usage and frequency of blood draws decreased. By the end of the intervention period, there was also a decrease in the number of CBCs ordered.
Conclusions: Inflammatory markers were often being obtained in multiples despite evidence showing it provides no benefit to patient diagnosis or management. Ordering rates were variable between providers. There was also variation based on patient diagnosis with highest rates amongst conditions with no or still developing evidence-based guidelines. Our quality initiative was associated with a significant reduction in the redundant use of inflammatory markers.