Background: There were approximately 46,000 opioid overdose deaths in 2017. It is known that opioid overdose risk is increased in patients with a diagnosis of substance use disorder, prior opioid overdose, and high suspicion of risk as assessed by clinical teams. The Risk Index for Overdose or Serious Opioid-Induced Respiratory Depression (RIOSORD) is a validated screening tool for quantifying risk of prescription opioid-induced respiratory depression in both inpatient and outpatient populations. In addition, patients with opioid use disorder, alcohol use disorder, and stimulant use disorder all have increased risk of opioid overdose, as well as patients who have had a prior opioid overdose. Although factors that increase risk of opioid overdose are known, systematic approaches to quantifying at-risk populations and providing evidence-based interventions are often lacking in inpatient populations.
Purpose: We developed a systematic approach for proactively identifying inpatients at risk of opioid overdose and providing evidence-based interventions to mitigate risk.
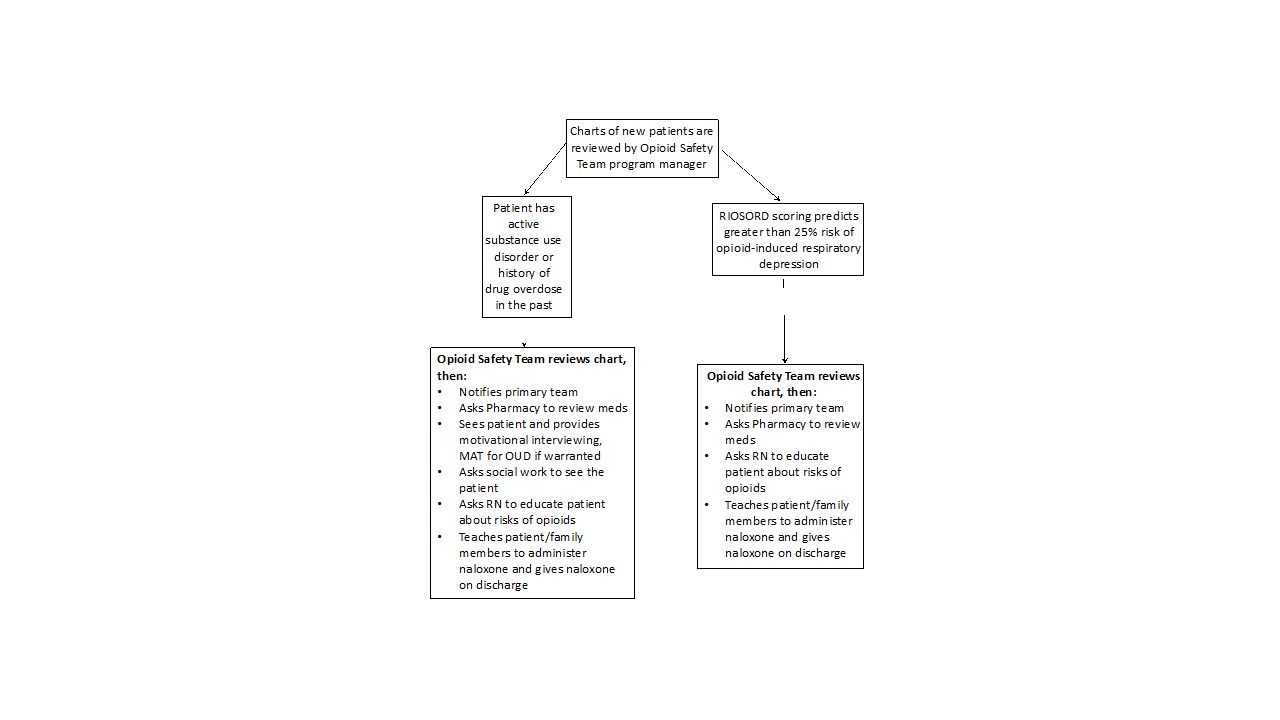
Description: Our intervention identified patients at high risk of opioid overdose during hospitalization and within two weeks of hospital discharge. Every morning, a program manager screened a subset of patients on a Hospital Medicine service for risk of opioid overdose by calculating a RIOSORD risk score and assessing for substance use disorders, previous opioid overdose, and high clinical suspicion for overdose. Patients who were screened as having greater than 25% risk of opioid overdose by RIOSORD or screened positive for any of the other risk factors were seen by a member of the Opioid Safety Team (OST) staffed by one hospitalist and one Nurse Practitioner. The OST provider reviewed the chart, contacted the primary team to inform them of the increased risk, and consulted a pharmacist to conduct a medication review to assess if any medications could be changed, such as benzodiazepene or opioid dosages. In addition, if the patient screened positive for a substance use disorder, a member of the OST saw the patient, and provided motivational interviewing and medication-assisted treatment (buprenorphine or methadone) as needed. At the end of a three-week period, of 89 patients screened, 29 (26%) patients screened positive for increased opioid overdose risk, and 19 patients were seen by a member of the OST. Of the 19 seen by the OST, 16 had a substance use disorder. The OST recommended initiation of a medication (naloxone, methadone or buprenorphine) to mitigate overdose risk in 18 of the 19 patients seen in person.
Conclusions: A system for screening patients for risk of opioid overdose can be developed and lead to changes in management of inpatients. This system is conducive to automation, given that most of the information that informs the screening tool can be found in the electronic medical record. Developing an automated tool that identifies at-risk patients is a potentially powerful next step for mitigating opioid overdose risk.