Background: Delirium, an acute cognitive disturbance prevalent in up to 58% of older hospitalized adults, poses serious health risks, longer hospital stays, and increased mortality (1). Identifying and screening for delirium is hindered by barriers such as limited awareness, inadequate education, and lack of prioritization among healthcare providers. This project aimed to gauge opportunities to improve care of patients with or at risk of developing delirium by surveying hospitalist and emergency medicine providers through the lens of the 4Ms of older adult care (mobility, medication, mentation, what matters) (2).
Methods: An anonymous survey was distributed to physicians (attendings, fellows, and residents) and advanced practice providers (nurse practitioners and physician assistants) at an academic medical center’s Internal Hospital Medicine (IM) (N=157) and Emergency Medicine (EM) (N=93) departments via Redcap. The survey assessed knowledge and attitudes about delirium identification, management, and prevention. Professional demographic information and free text responses were also collected.
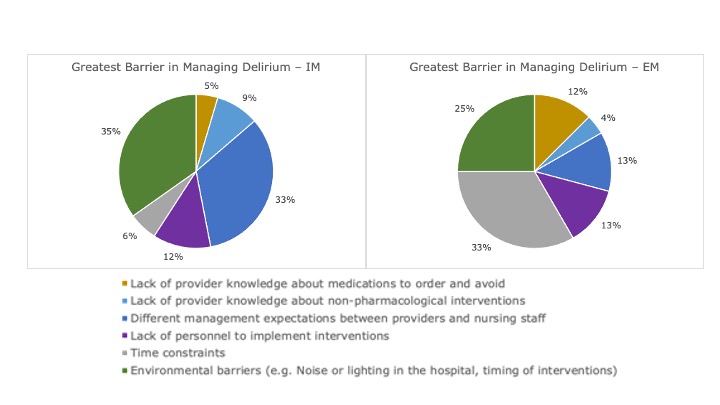
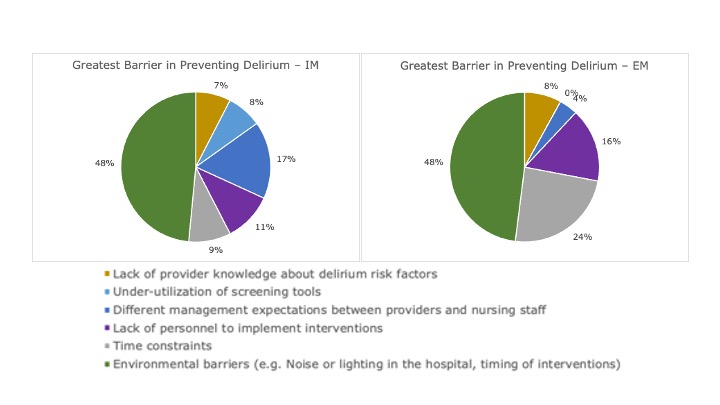
Results: Of the 250 surveys distributed, 92 were completed (36.8% response rate). Overall, most respondents were in the IM department (72.8%) and were resident physicians (53.2%). 9 (9.8%) indicated that they had additional training related to caring for older adults. Regarding delirium knowledge, providers showed adequate knowledge base (89.2% correct answers); however, 20 (21.7%) respondents did not identify inattentiveness as a possible indication of delirium and 16 (17.3%) did not identify mobility as a possible method for managing delirium. Providers rated themselves as more confident in identifying than managing delirium (96.8% vs. 90.5% with “Fair” or above). No providers believed that delirium is impossible to prevent, but 87% think that it is “sometimes”. 66% of providers reported that discerning delirium from other illnesses made it difficult to detect, and 31% thought that lack of medical prioritization was a barrier to care. While both IM and EM named environmental barriers and time constraints as major barriers to addressing delirium, 32.8% of IM providers pointed to differing management expectations between providers and nursing staff whereas EM providers frequently cited medication knowledge and lack of personnel. Both departments suggested systems-based solutions as an ideal starting point, even in the free text section.
Conclusions: Our survey revealed an overall good understanding of delirium identification, management, and prevention, as well as relatively high confidence and positive attitude in providers regarding the importance in addressing delirium. Seeing a plurality of providers within both departments identify common barriers and potential solutions suggests that there are potential next steps to improve patient outcomes. There is a salient need to create systematic solutions to help mitigate the incidence and prevalence of delirium in the inpatient hospital setting and emergency room.