Background: Survivors of critical illness, such as acute respiratory distress syndrome (ARDS) requiring invasive mechanical ventilatory support in an intensive care unit (ICU), commonly experience prolonged morbidity in multiple health domains: psychological distress, functional debility, cognitive impairment, and poorer quality of life. This resulting morbidity is now recognized broadly as post-intensive care syndrome (PICS). COVID-19 ICU survivors are at high risk for PICS.
Methods: This study aims to describe functional, psychiatric, and quality of life outcomes of COVID-19 ARDS adult survivors who required mechanical ventilation in a safety-net hospital. Subjects were referred months after discharge to a designated physiatry clinic and established care in 2021. They received routine physiatry care and psychological screening, using Generalized Anxiety Disorder 7 (GAD7), Patient Health Questionnaire 9 (PHQ-9), Post-traumatic stress disorder Checklist-Civilian (PCL-C), a PICS survey, and Satisfaction with Life Scale (SWLS). Data was collected retrospectively from the electronic medical record, and patient characteristics were summarized using descriptive analysis.
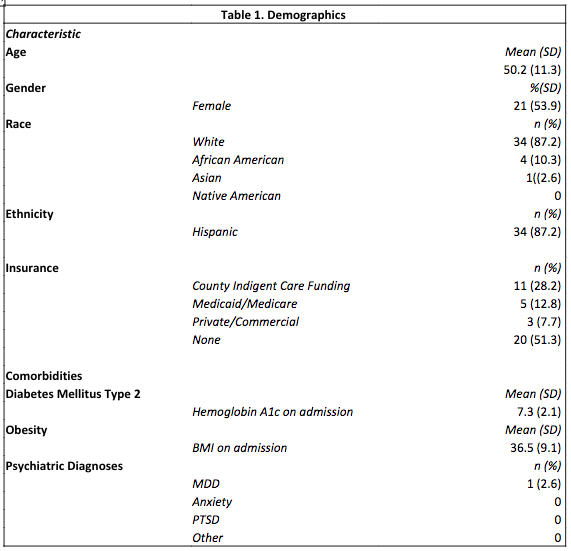
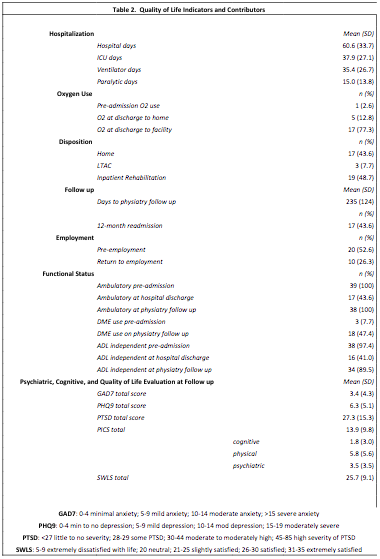
Results: 39 patients met inclusion criteria. The mean age was 50.2 years (SD 11.3), 53.9% female, and 87.2% identified as white, all of which were Hispanic. 20 patients were unfunded prior to hospitalization, and 11 had charity funding. The median hospital length of stay (LOS) was 46 days (IQR 37-80) with 29 (18-52) ICU days and 10 (6-21) days of paralytics. 17 patients were discharged home, 19 to inpatient rehabilitation, 3 to long-term assisted care facility, and 17 were readmitted within 12 months. 22 patients required supplemental oxygen at discharge. The median days to establish care in physiatry clinic was 220 (138-337). All patients were ambulatory previously; only 17 were ambulatory at hospital discharge and 38 at physiatry follow up. 20 patients were previously employed; 10 were employed at follow up. 38 patients were previously independent in activities of daily living (ADL), 16 at discharge, and 34 by follow up. Mean survey scores were GAD7 3.4 (4.3), PHQ-9 6.3 (5.9), PCL-C 29.7 (13.8), SWLS 25.7 (9.1). 5 (12.8%) patients reported subjective cognitive deficits.
Conclusions: While most of our COVID-19 critical illness survivors regained community level ambulatory and ADL independence, 50% fewer patients were employed at follow up, suggesting unmeasured persistent functional debility or other health domain deficits, consistent with other populations of critically ill ARDS survivors. Only one patient was identified as having a pre-existing psychological disorder (depression). The survey results suggest new mild depression and some to moderate post-traumatic stress disorder symptoms. Quality of life fell between slightly satisfied to satisfied. While the study lacked formal cognitive assessments, the results suggest at least mildly persistent cognitive symptoms in 12.8%. Some studies suggest higher rates of cognitive symptoms in other COVID-19 populations and other ICU survivors. This cohort is unlikely representative of all critically ill COVID-19 ARDS survivors as the sample size is small and specific to our safety-net hospital. Remarkable health resiliency is demonstrated, though morbidity persists requiring ongoing care. More work on prevention and appropriate treatment of PICS is warranted for all survivors of critical illness.