Background: An observation unit is a short-stay, strictly protocolized, low-acuity unit created by and managed by emergency physicians. This traditional model is evolving given the increase in complexity of comorbidities and socioeconomic challenges of patients. Although patients may present with low acuity issues, they do not always meet the inclusion/exclusion criteria for the Emergency Department (ED)–run clinical decision unit (CDU)/observation unit. Grady Memorial Hospital (GMH) has created a hospitalist-run short-stay unit, known as the Inpatient Observation Unit (IOU), that is more liberal in criteria to capture this patient population, decompress the ED, and improve patient throughput.
Methods: The IOU is a 10-bed telemetry and intermediate care capable short-stay unit that opened mid-October 2022. It is a closed unit located adjacent to the ED staffed by one hospitalist and one Advanced Practice Provider. The ED calls the IOU hospitalist directly for possible admission. Patient selection and admission is determined by the IOU hospitalist’s judgement of whether the patient can be discharged within 48 hours and an internal tip sheet with exclusion criteria. The patient can be assigned either “inpatient” or “observation” status, depending on the medical necessity.
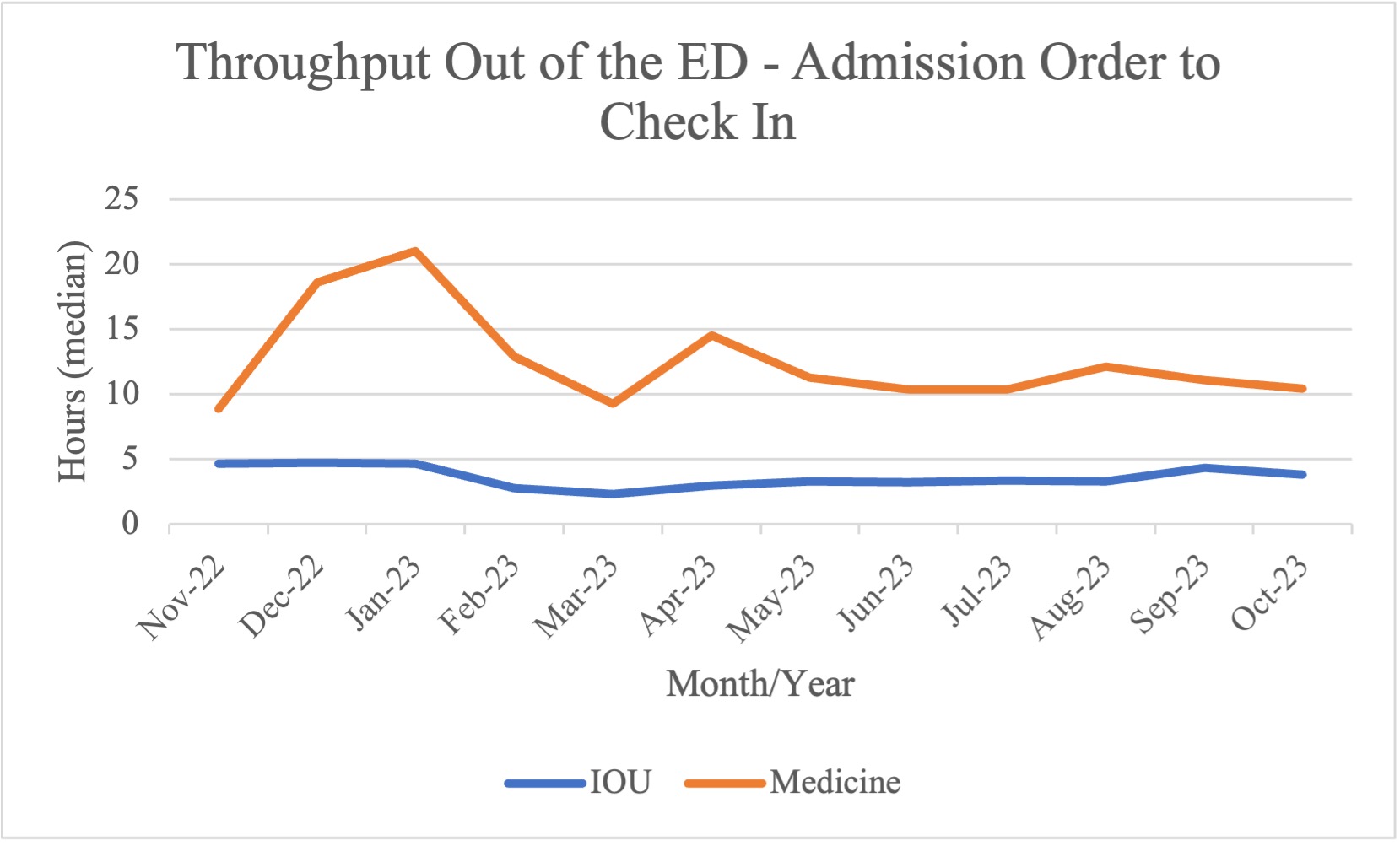
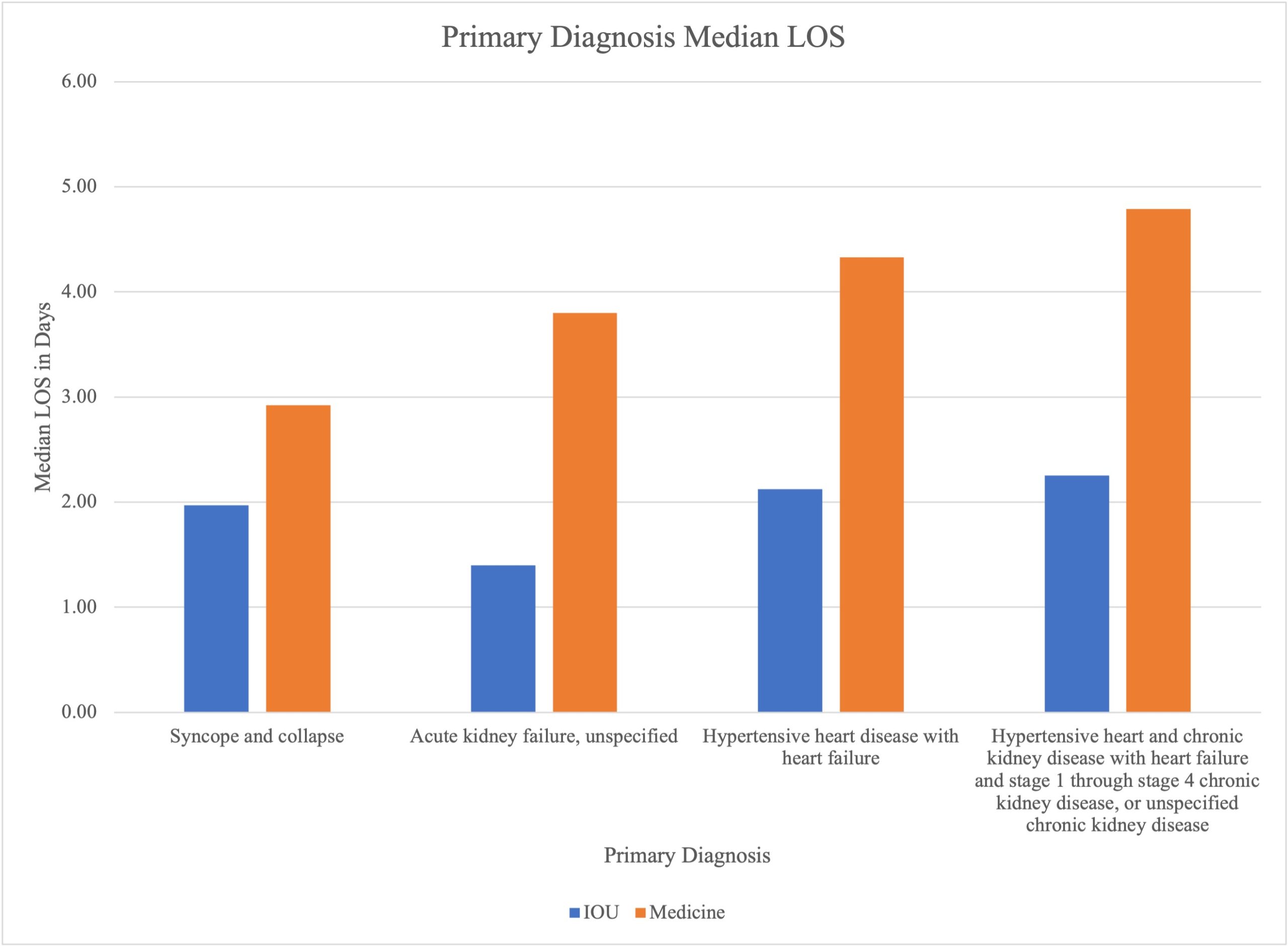
Results: Our analysis of preliminary data from November 2022 to October 2023 show a median time from admission order to exiting the ED of 207 minutes (3.45 hours) for IOU patients versus 720 minutes (12 hours) for general medicine patients, demonstrating a 71.25% efficiency gain. When comparing length of stay (LOS) of common primary diagnoses among IOU patients versus non-IOU patients admitted with the same primary diagnosis, “syncope and collapse” LOS for IOU patients is 1.97 days versus medicine patients’ 2.92 days; “acute kidney failure” LOS for IOU patients is 1.40 versus 3.80 for medicine patients; “hypertensive heart disease with heart failure (HF)” for IOU patients is 2.12 versus 4.33 for medicine patients; and “hypertensive heart and chronic kidney disease (CKD) with HF and stage 1 through stage 4 CKD” for IOU patients is 2.25 vs 4.79 for medicine patients. The IOU increased utilization for observation status patients by about 19.25%: the mean number of patients in observation status was 108 before implementation of the IOU (January-September 2022) and 133 after implementation (November 2022-October 2023).
Conclusions: The hospitalist-run short-stay IOU is an innovative solution to capture the patient populations that are low acuity but do not meet the criteria for the CDU. This unit has been largely successful in decompressing the ED and progression of care and LOS of common primary diagnoses, showing improved patient throughput compared to other medicine teams. The IOU provides necessary testing priority to patients quickly and has dedicated resources to facilitate patient progression. The IOU also increased utilization of observation status, which we hypothesize that this change will help to decrease insurance denials and improve reimbursement. Next steps include finding a process to capture more of the short-stay patients directly from the ED to further expedite patient care and to expand and update our evaluation data analysis.