Background: Medication errors occur frequently at transitions of care and lead to significant patient harm. Robust medication reconciliation practices can mitigate these errors, but this process is complex and time-consuming. One of the conclusions of the first Multi-center Medication Reconciliation Quality Improvement Study (MARQUIS1) was that pharmacist team involvement in medication reconciliation is a key component to improving the quality and safety of the process. Because pharmacist resources are often limited, one goal of sites in the second MARQUIS study was to efficiently deploy these limited resources to those patients at highest risk of suffering harm.
Purpose: We describe the efforts of two health systems in MARQUIS2, the University of California at San Diego (UCSD) and Oregon Health Science University (OHSU), to improve inpatient medication reconciliation efficiency by targeting pharmacy team resources to patients at highest risk for medication error-related harm using an automated risk-stratification tool linked to an EHR.
Description: UCSD developed the risk score based on the literature and data readily available from its EHR, including total number of preadmission medications and number of high-risk medications in the patient’s outpatient profile. Scores > 7 were considered high risk. Scores > 4 were considered moderate risk. Pharmacy technicians at UCSD use this tool to prioritize medication histories for patients as follows: 1) ED patients with admission status and a moderate or high risk score 2) high risk patients who were admitted the previous day 3) ED patients with a high risk score regardless of admission status and 4) ED patients with no home medications recorded in the EHR profile.
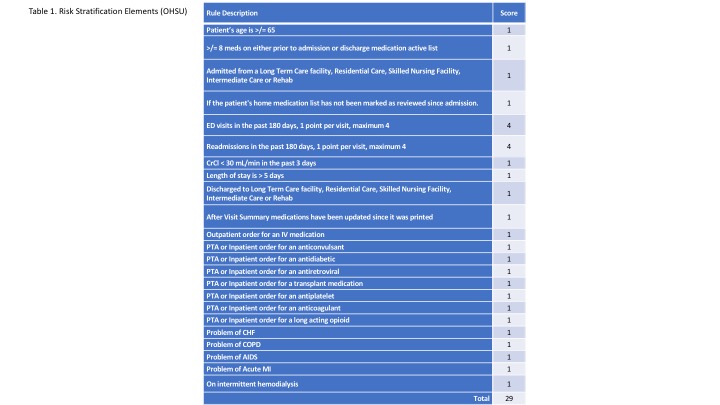
OHSU adopted the risk stratification scoring framework from UCSD’s successful experience. OHSU modified the risk stratification tool to customize for unit-based pharmacist staffing and focus on admission medication reconciliation (Table 1). The scoring threshold triggering pharmacist intervention was also adjusted according to the capacity of each unit pharmacist.
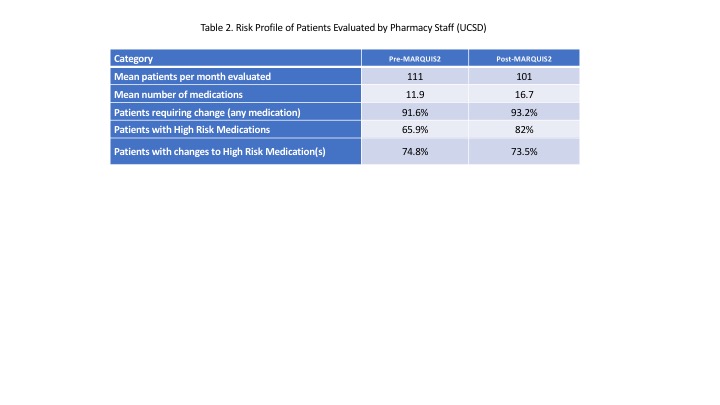
Conclusions: Upon implementing the risk score tool in September 2016, pharmacy staff at UCSD performed medication histories on patients with more complex medication regimens (Table 2). The implementation of the scoring tool at OHSU was similarly successful. Both sites plan to continue to refine the scoring tool and their workflows. We intend to spread the tool to other Epic-using MARQUIS2 sites and eventually to other health and hospital systems.