Background: Typical solutions to incorporating provider input into discharge planning often rely on one-way communication mechanisms and data entry that is not dynamic (i.e. providers estimate day of discharge in advance). We are designing a discharge readiness tool to be integrated into our current electronic health record (EHR), Epic Systems-Verona Wisconsin, that allows providers to more easily communicate three useful pieces of information: estimated date of discharge, whether this is a possible or definite discharge date, and the barriers to discharge from the providers’ perspective. This information will be disseminated to other care team members using the EHR to enhance prioritization of tests, interventions, and bed flow. Stakeholder engagement is imperative to ensure our discharge readiness tool is successfully integrated into existing the provider and ancillary department workflows such that clinical staff, both hospitalists and ancillary providers, will this tool with every patient.
Purpose: We aim to describe the engagement strategy we employed to develop and modify an innovative EHR-based discharge communication tool. Using a pragmatic approach to ensure that our tool is based on a practical rather than theoretical foundation, we assessed current functionality of existing processes for documenting discharge readiness and directing discharge planning work by gathering stakeholder feedback. Utilizing this information and our previous work on barriers to earlier discharge, we designed an EHR discharge readiness tool. After creating a low-fidelity mock-up of the discharge readiness tool functionality, we presented this tool to our stakeholders, iteratively modifying the tool based on feedback received about functionality and integration into their existing workflows.
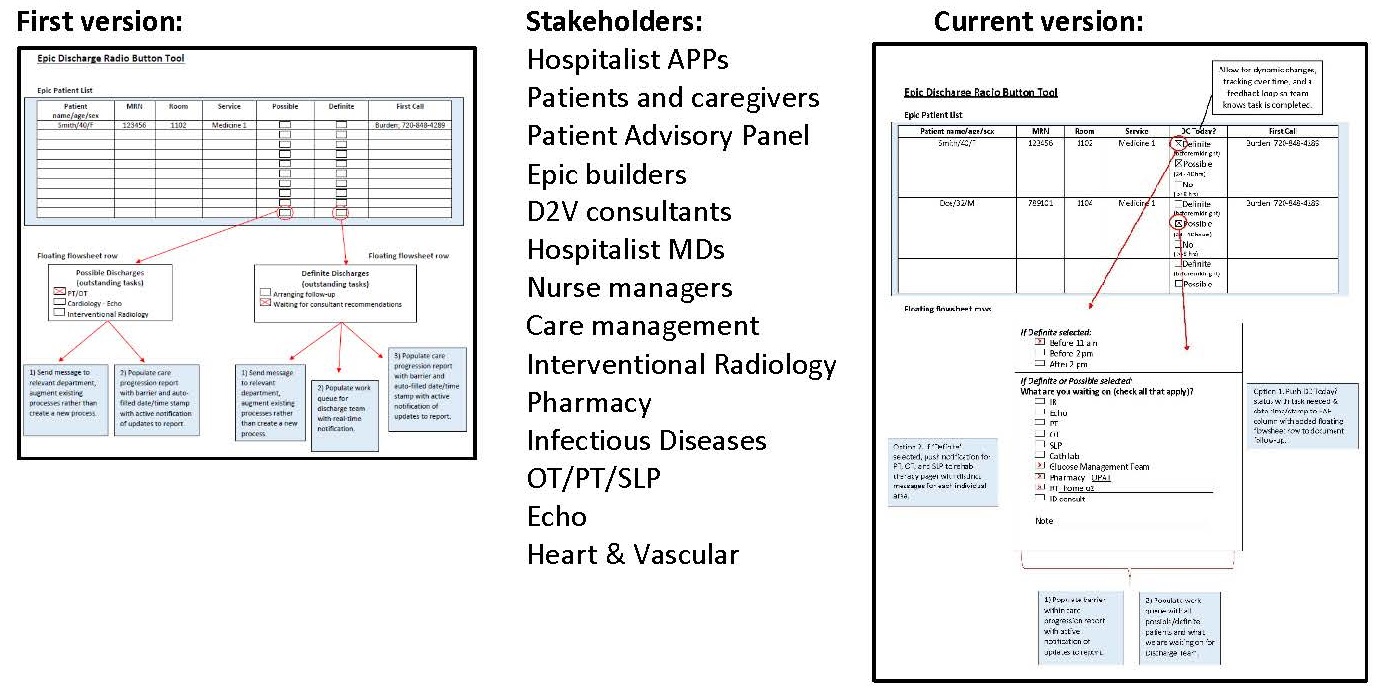
Description: The low-fidelity mock-up has been modified 11 times, following conversations with recently discharged patients or their families, a patient advisory panel, clinical design experts, Hospital Medicine APPs and MDs, nurse managers, care management staff, IR, pharmacy, OP, PT, SLP, Cardiac Cath lab, Echo, and RT. We also applied a novel engagement strategy, Brainwriting Premortem, to specifically engage stakeholders in identifying potential barriers that we might encounter when implementing the discharge readiness functionality in the EHR whereby participants are asked to write down all the reasons each of them could think of that would have caused this tool to fail. The pages were collected from each participant and collated later for consideration by the project team.
Conclusions: By utilizing a deliberate and collaborative stakeholder engagement process, we have obtained commitment to testing our EHR discharge readiness tool from 100% of key stakeholders. Before implementing this tool for clinical use, we will present the tool in the pre-production EHR testing environment for stakeholder approval. In addition, we will use a cognitive walkthrough process to assess the usability of our discharge readiness tool by observing whether a new user can easily carry out the tasks required. We use these data to modify the design of the tool if needed. We will then undertake an extensive evaluation of the tool in clinical use from a multi-stakeholder perspective.