Background: Urinary tract infection (UTI) and community acquired pneumonia (CAP) are the two most common infections treated in hospitalized patients and are often inappropriately diagnosed. Due to myriad factors—including diagnostic uncertainty—patients are commonly inappropriately diagnosed with UTI or CAP in the emergency department (ED). Antibiotics may be continued throughout the hospitalization even if new information is available to refute the initial infectious diagnosis (i.e., diagnostic momentum). Here, we characterized the variation in diagnostic momentum across conditions and hospitals and identify hospital characteristics associated with diagnostic momentum.
Methods: This retrospective cohort study includes patients hospitalized in 68 Michigan hospitals between 1/1/2018-2/15/2023 who were “inappropriately diagnosed” and treated for UTI or CAP. Consistent with national guidelines and National Quality Forum (NQF)-endorsed quality metrics, we considered patients inappropriately diagnosed with UTI if they lacked signs or symptoms of UTI (i.e., had asymptomatic bacteriuria) and to be inappropriately diagnosed with CAP if they did not meet diagnostic criteria for CAP (≥2 signs/symptoms plus radiographic criteria). Our primary outcome was the percentage of patients inappropriately diagnosed with CAP or UTI in the ED who had diagnostic momentum, defined as antibiotic duration of ≥3 days (including discharge antibiotics).
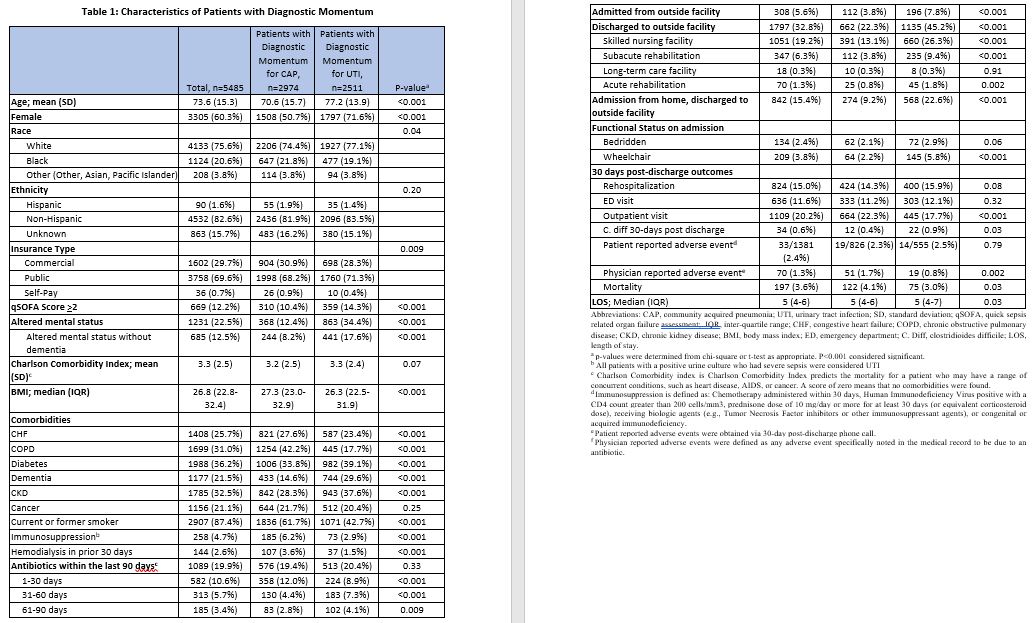
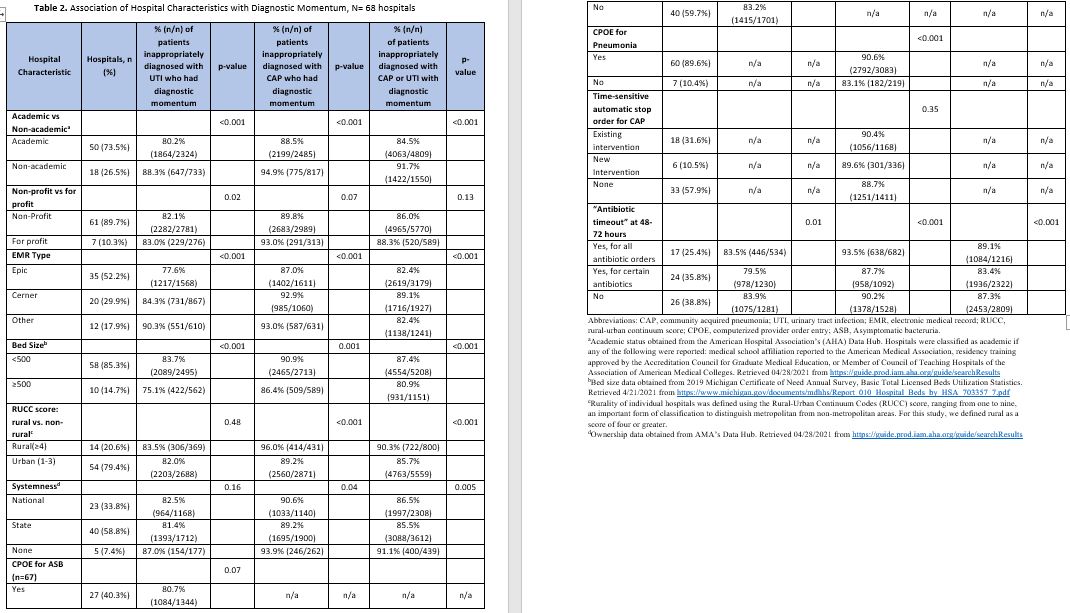
Results: Between 1/2018 – 2/15/2023, there were 40,212 patients treated for CAP and 32,403 patients treated for UTI across 68 hospitals within the Michigan Hospital Medicine Safety Consortium. Of those, 11.8% (4755/40212) of patients treated for CAP and 18.5% (5991/32403) of patients treated for UTI were inappropriately diagnosed. Of those with antibiotics started by an ED provider, 90.1% (2974/3302) of CAP and 82.1% (2511/3057) of UTI patients met our definition of diagnostic momentum (i.e., antibiotic duration ≥ 3 days). Compared to patients without diagnostic momentum, those with diagnostic momentum were less likely to be women and more likely to have altered mental status (details in Table 1). Hospitals varied considerably in their percentage of patients with diagnostic momentum, from 53.8%-100% for CAP and from 54.5%-100% for UTI. Diagnostic momentum for CAP was correlated with diagnostic momentum for UTI at the hospital level (R^2=0.127, p=0.005). Smaller, non-academic, rural hospitals that did not belong to a system of hospitals as well as those with Cerner (vs. Epic) had more diagnostic momentum whereas stewardship interventions did not appear to have a large impact on diagnostic momentum (details in Table 2).
Conclusions: Diagnostic momentum for hospitalized patients inappropriately diagnosed with infections is common. Hospitals with less diagnostic momentum for CAP tend to also have less diagnostic momentum for UTI and vice versa. Hospitals with more resources have less diagnostic momentum but no specific stewardship interventions appeared to explain this difference. New interventions may be needed to combat diagnostic momentum in patients started on antibiotics in the emergency room.