Background: With the coronavirus disease 2019 pandemic, the need for telemedicine is growing rapidly worldwide. The development and improvement of remote physical examination systems, especially remote cardiopulmonary auscultation are required to facilitate telemedicine. A system combining an electronic stethoscope and Bluetooth connectivity is a promising option for remote auscultation in hospitals and clinics. However, the utility of such systems remains unknown.
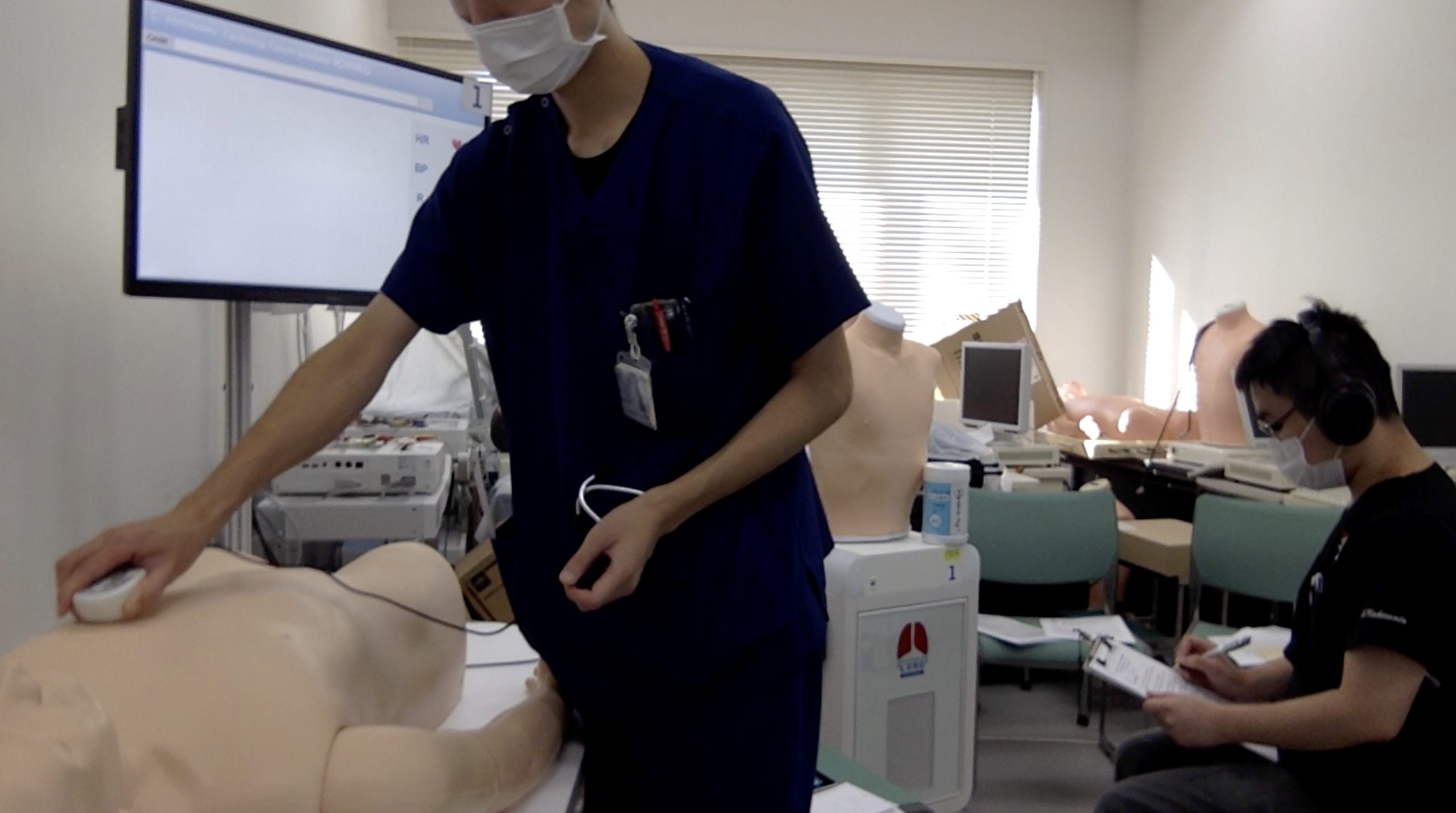
Methods: This study was conducted to assess the utility of real-time cardiopulmonary auscultation, using a Bluetooth-connected electronic stethoscope compared to that of classical auscultation, using a lung simulator and a cardiology patient simulator. This was an open-label randomized controlled trial, including senior residents and faculty in the department of general internal medicine of a university hospital. The only exclusion criterion was a refusal to participate. This study consisted of lung auscultation part and the heart auscultation part. Each part contained a tutorial session and a test session. All participants attended the tutorial session, in which they listened to 15 sounds on the simulator using a classic stethoscope and were told the correct classification. Thereafter, participants were randomly assigned to either the real-time remote auscultation group (intervention group) or the classical auscultation group (control group), for the test sessions. In the lung and heart test sessions, participants had to classify a series of ten lung sounds (two different normal sounds, three different wheezes, rhonchi, coarse crackles, fine crackles, pleural rubs, and stridor) and ten heart sounds (two different normal sounds, two different S3, aortic stenosis, aortic regurgitation, mitral stenosis, mitral regurgitation (twice), and atrial fibrillation), respectively. The intervention group listened to the sounds remotely, using the electronic stethoscope, a Bluetooth transmitter, and a wireless, noise-canceling, stereo headset. The control group listened to the sounds directly using a traditional stethoscope. The primary outcome was the test score, and the secondary outcomes were the rates of correct answers for each sound.
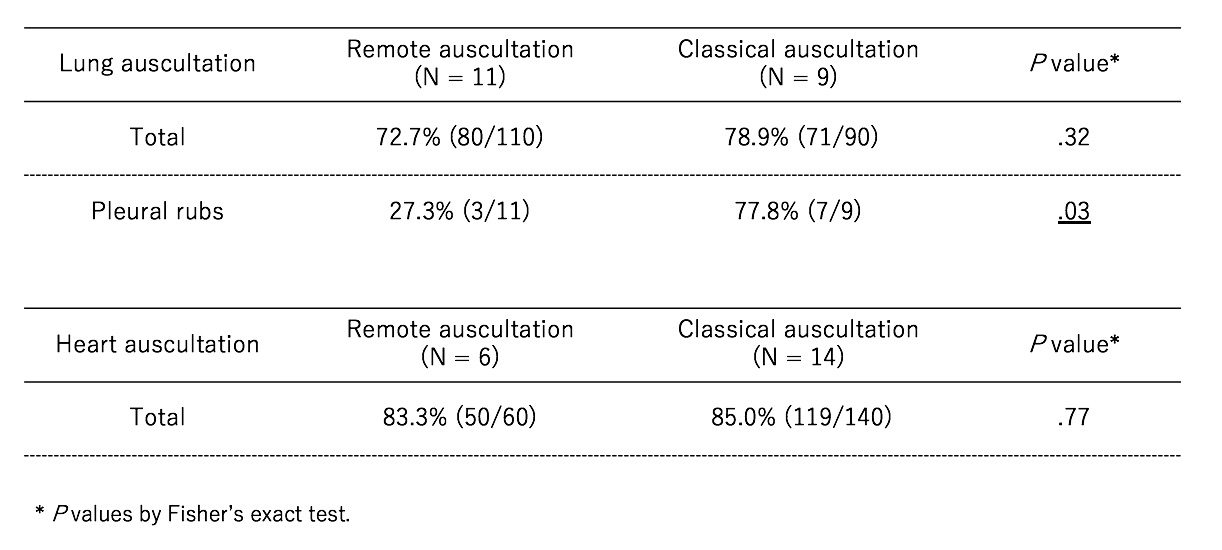
Results: In total, 20 participants were included; eleven and nine were assigned to the intervention and control groups, respectively. There was no difference in age, sex, and years from graduation between the two groups. The overall test score of lung auscultation in the intervention group (80/110, 72.7%) was not different from that in the control group (71/90, 78.9%) (P=0.32). The only lung sound for which the correct answer rate differed between groups was that of pleural friction rubs (P<0.05); it was lower in the intervention group (3/11, 27%) than in the control group (7/9, 78%,). The overall test score of heart auscultation in the intervention group (50/60, 83.3%) was not different from that in the control group (71/90, 85.0%) (P=0.77). There was no heart sound for which the correct answer rate differed between groups.
Conclusions: The utility of a real-time remote cardiopulmonary auscultation system using a Bluetooth-connected electronic stethoscope was comparable to that of direct auscultation using a classic stethoscope, except for classification of pleural friction rubs. This means that most of the real world’s essential lung and heart sounds could be classified by a real-time remote auscultation system using a Bluetooth-connected electronic stethoscope.