Background: The American healthcare system is focused on promoting value; providing high quality care while paying close attention to associated costs. Studies have shown that admission to a teaching hospital is associated with better outcomes, reduced mortality, compared to nonteaching hospitals. It is not known whether the value proposition at academic hospitals is worthwhile for routine conditions in addition to more specialized conditions. Because delirium is a common and costly condition among hospitalized patients and approaches to care are not standardized, this study set out to explore distinctions in clinical and process outcomes for patients with delirium between teaching and nonteaching hospitals.
Methods: We used the 2014 Nationwide Inpatient Sample database to identify adults >= 18 years who were admitted with a principal diagnosis of delirium (by ICD-9 code). The primary outcome was in-hospital all-cause mortality. Secondary outcomes were discharge status and several measures of health care resource utilization: length of stay (LOS), total hospitalization charges, total hospitalization costs, neurological workup, and multiple procedures performed during hospitalization. Multivariable logistic regression analysis models were used to adjust for potential confounders such as patient age, sex, race, median yearly income in the patient’s zip code, insurance, comorbidities (Charlson Comorbidity Index for administrative data), hospital location (rural or urban), geographic region (Northeast, Midwest, West, or South), control/ownership of hospital, and hospital bed size. All tests used a significance level of P<0.05.
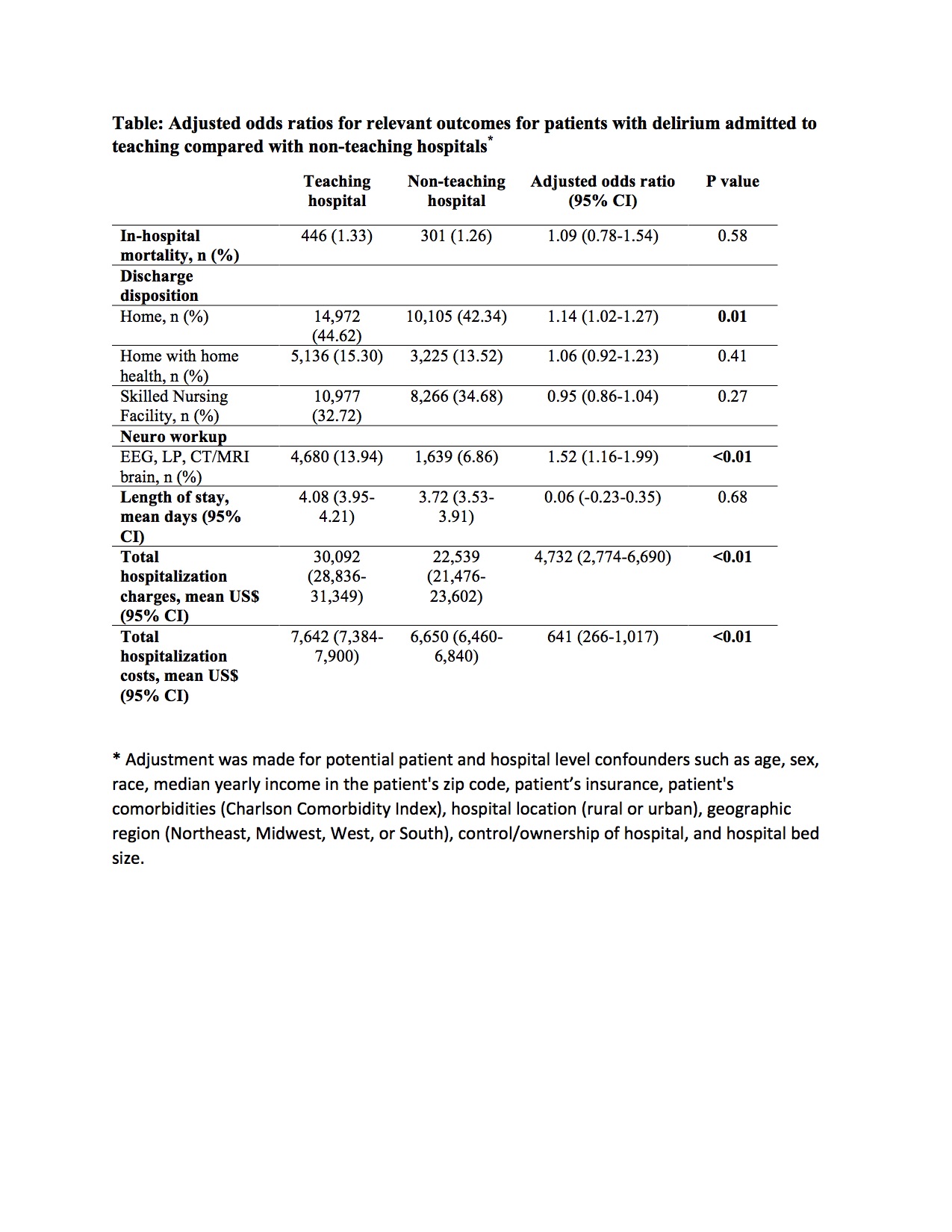
Results: In 2014, out of 57,460 adult patients admitted to hospitals with delirium in the analysis, 58.4% were hospitalized at teaching hospitals and the remainder (41.6%) to nonteaching hospitals. The in-hospital mortality of delirium patients at teaching hospitals was 1.33% (95% CI 1.08% – 1.63%), and 1.26% (95% CI 0.97% – 1.63%) at nonteaching hospitals. The mean LOS was 4.08 days (95% CI 3.95-4.21) at teaching hospitals, and 3.72 days (95% CI 3.53-3.91) at nonteaching hospitals. The mean total hospitalization charges were $30,092 (95% CI 28,836-31,349) at teaching hospitals, and $22,539 (95% CI 21,476-23,602) at nonteaching hospitals. After adjustment for confounders, total hospitalization charges and costs were statistically significantly different between the hospital types – with nonteaching providing less expensive care (Table).
Conclusions: Patients with delirium admitted to nonteaching hospitals realized comparable clinical and process outcomes to those cared for at teaching hospitals; achieved at lower costs. These data suggest that nonteaching hospitals may be providing enhanced value for patients presenting with delirium.