Background: Since the start of the COVID-19 pandemic, racial and ethnic minorities have experienced disparities in infection rates, hospitalization, and death. Monoclonal antibodies (Mab) decrease hospitalization when given to ambulatory non-severe high-risk patients within 10 day of symptom onset. Disparities in care related to Mabs are not well understood. We describe experience from Mab infusion center operated by hospital based team at Baltimore Convention Center Field Hospital (BCCFH).
Methods: All eligible patients referred to BCCFH infusion center from 1/4/2021 to 5/14/2021 were included. BCCFH started as a COVID overflow inpatient service. Because of lack of ambulatory space in existing health system to treat COVID patients, the inpatient team created space and capabilities to provide ambulatory Mab infusions. Treatment and free transportation were provided with no out-of-pocket payment. The data for final scheduling and treatment status for patients were obtained. Final status of “Refused Treatment” or “Cancelled” was categorized as mAb “Hesitancy” because they were linked with doubts about the treatment. All final statuses where patients did not receive treatment, including those related to Hesitancy, were considered “Underutilization.” Final status of treatment at BCCFH or elsewhere was categorized “Appropriate Utilization.” Racial disparities were assessed using logistic regression, adjusted for gender, age, and poverty rate in zip code of residence (using American Community Survey data), to compare odds by race for each final status, hesitancy, underutilization, and appropriate utilization.
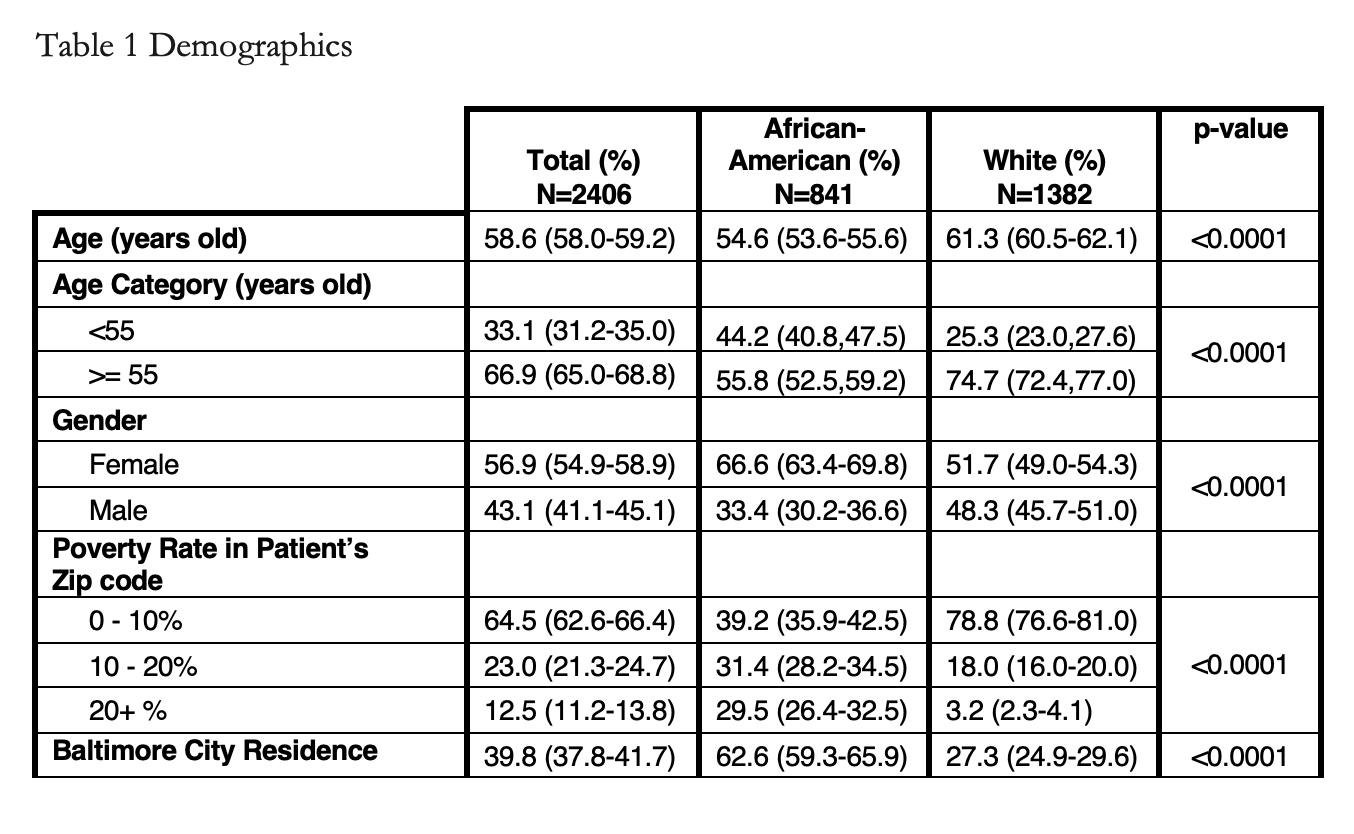
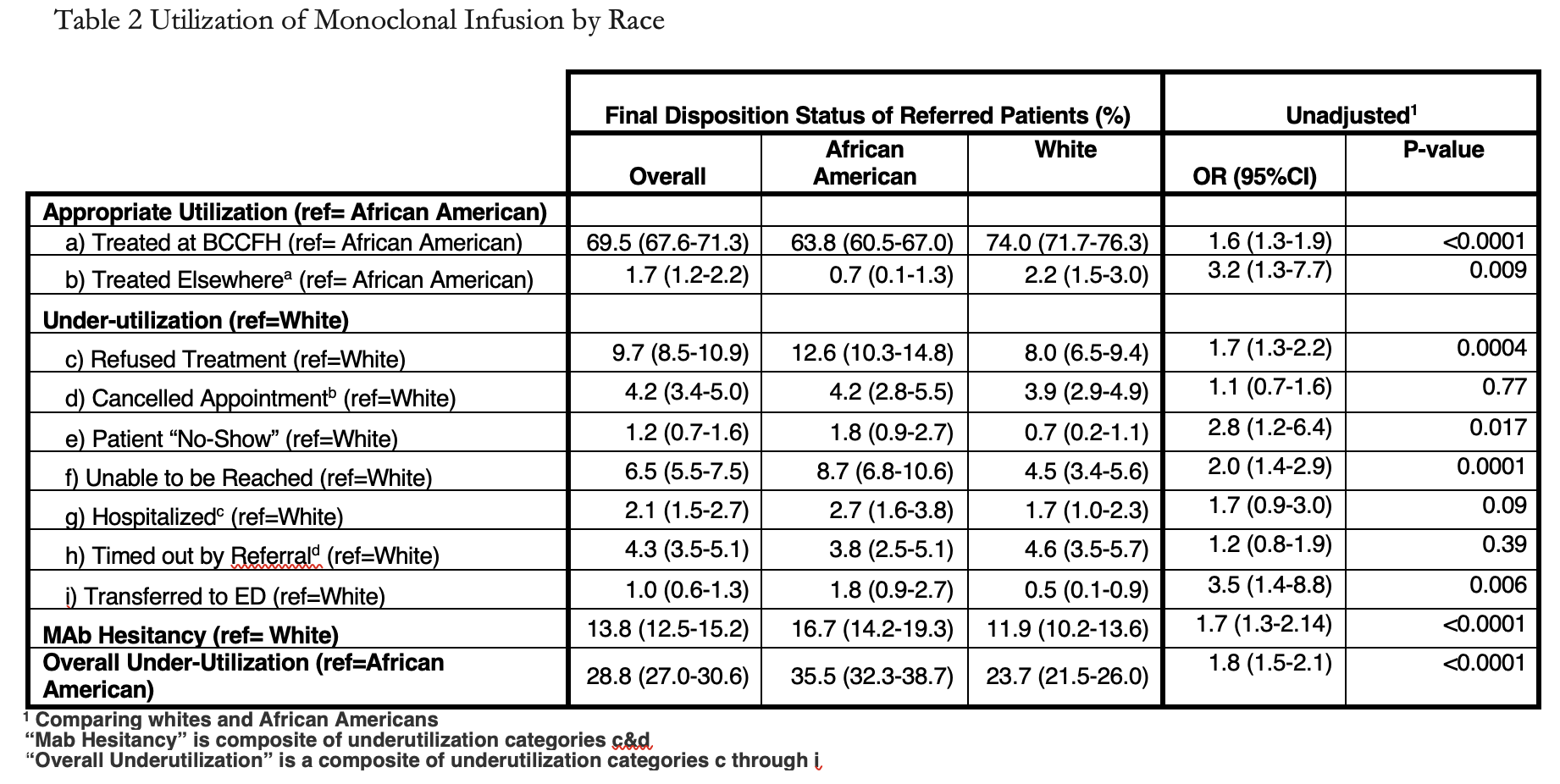
Results: Among 2406 eligible patients referred, 57.4% were white, 35% were African American. Their mean age was 54.6. African Americans were younger, more often female, city residents and from high poverty zip codes (Table 1). Overall, 69.5% of referred patients were treated at BCCFH, with 74% of referred whites and 63.8% of referred African American receiving mAb. African Americans more often underutilized mAb treatment (OR1.8; 95% CI: 1.5, 2.1). Mab hesitancy accounted for 48.0% (95% CI, 44.3-51.7) of underutilization and African Americans more often missed treatment opportunities because of monoclonal hesitancy (OR 1.7; 95% CI: 1.3-2.1). African Americans more often refused treatment, cancelled the appointment, were unreachable, were hospitalized before the appointment, or were transferred to the Emergency Department on arrival. Overall, whites had greater odds of being treated at BCCFH (OR 1.6; 95% CI, 1.3-1.9) or another infusion site (OR 3.2; 95% CI, 1.3-7.7). (Table 2).
Conclusions: Despite overcoming barriers related to timely COVID testing and seeing a physician quickly to be referred within 10 days of symptoms and apparently agreeing to mAb as evidenced by provider referral, Africans Americans underutilized this treatment relative to whites. Nearly half of the eligible patients were untreated because they declined treatment or cancelled after setting an appointment. We have categorized this as hesitancy and African American had 1.7 the odds as whites of being hesitant. The refusal is not likely to be due to African Americans feeling better prior to the treatment, since they were the sicker group, as evidenced by higher rates of missed treatments because of hospitalization or pretreatment decompensation in the infusion center. Future novel treatments should address hesitancy in underserved groups similar to efforts for COVID vaccination.