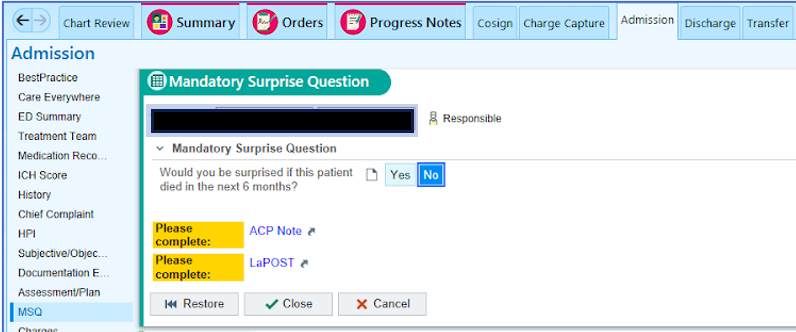
Background: Problem Definition: Inadequate Advance Care Planning conversations and documentation remain a persistent gap in healthcare delivery. Admitting patients to the inpatient service without explicitly exploring the ‘goals of care’ and ‘code status’ results in stressful moments for the patients, their families, and providers if the condition deteriorates and may result in providing care that does not align with the patient’s wishes and values.Aim Statement: Improve the Advance Care Planning “ACP” documentation by at least 20% in all patients admitted under the Family Medicine resident-led inpatient service.Plan: Introduce and normalize using the “Mandatory Surprise Question” or “MSQ”. The MSQ Is a feature built into the electronic health record (EHR) used in our hospital (Epic). The MSQ asks if you would be surprised if the patient died in the next six months. If the answer is “NO”, it prompts the completion of code status discussion and documentation.Problem characterizations:• Lack of structured education on the importance of ACP discussions and documentation• Time constraints provided the lengthy and challenging discussions, with the ACP conversations and documentation less prioritized
Methods: Methods: A Quasi-experimental study aimed to study the rates of ACP documentation pre- and post-interventionIntervention: A 15-minute educational session was conducted on the residents’ didactics day. We had an interactive discussion about the importance of ACP discussions and documentation. The residents were educated about the “Mandatory Surprise Question” feature and encouraged to normalize its use as an integral element in patient care. The session was followed by a mass email to the residents and faculty demonstrating the steps to answering the MSQ on the EHR. The intervention also included posters in the residents’ lounge as a reminder to use the MSQ.
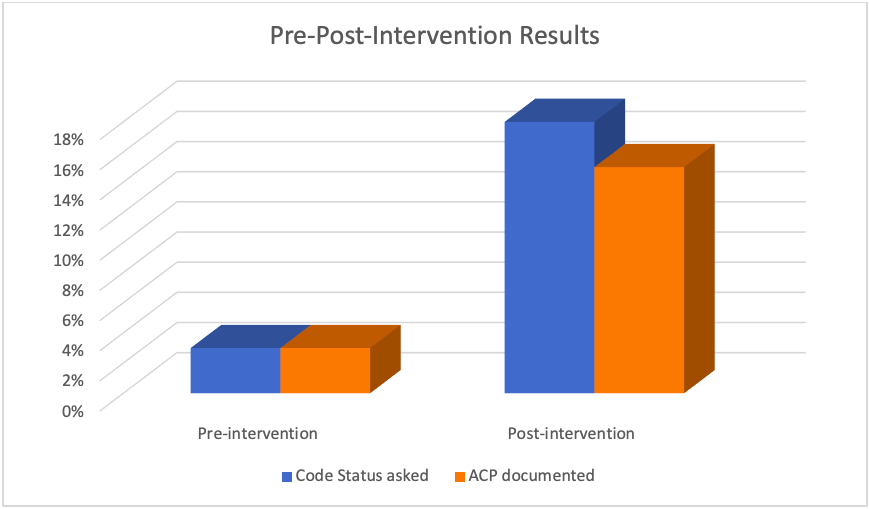
Results: Results: The pre-intervention data included the patients admitted to the service two weeks before the intervention. Similarly, the post-intervention data included the patients admitted to the service during the two weeks following the intervention.Baseline/Pre-intervention: 3% of the patients on service were asked about the code status and had ACP documentation during the hospital encounter.Post-intervention: 18% of the patients on service were asked about the code status, and 15% had ACP documentation during the hospital encounter.• Based on the residents’ feedback, a common challenge to achieving higher ACP documentation rates was the confidence level in carrying out a sensitive discussion. In the next PDSA, we will address the confidence in holding the discussions by arranging small group training sessions.• Another recognized challenge was the length of the discussions and the residents’ time constraints due to numerous duties. The ACP discussion and documentation were less prioritized among the clinical. Motivational interventions will be necessary as a future intervention to motivate the residents to prioritize ACP conversations and documentation.
Conclusions: • The study helps educate the residents and all healthcare providers regarding the crucial importance of ACP discussions and documentation.• Our intervention targeted the normalization of the MSQ use and carrying out ACP as an integral part of patient care. The study demonstrated a substantial increase in the rates of ACP documentation.• We plan to develop strategies for sustaining the change and achieving higher documentation rates by conducting training sessions.