Background: For 6 months in 2018, a major quaternary-care teaching hospital underwent closure of operating rooms (OR) and cardiac catheterization laboratory (CCL) due to flooding/sterilization issues and planned upgrades. Surgery and interventional cardiology trainees were reassigned to other teaching hospital sites of Yale School of Medicine, with the anticipated impact on Medicine/subspecialties not fully known. We report the effect of OR/CCL closure on education of non-surgery trainees, and on inpatient workload and hospital quality measures that have not been previously described.
Methods: Trainee Experience: Feedback was obtained by an electronic anonymous survey querying the effects of closures from 7/14/18-12/31/18 on education, professional development, day-to-day experience, work-related frustration/anxiety, and quality of patient care using a visual analog scale (-50 to +50) and free-text boxes. Student’s t-test or Mann Whitney U test compared survey results. Inpatient workload for Medicine/medical subspecialties and hospital quality measures: were compared with those in the same date period in 2017 and 2019, using negative binomial regression and maximum likelihood event count time series analysis on STATA.
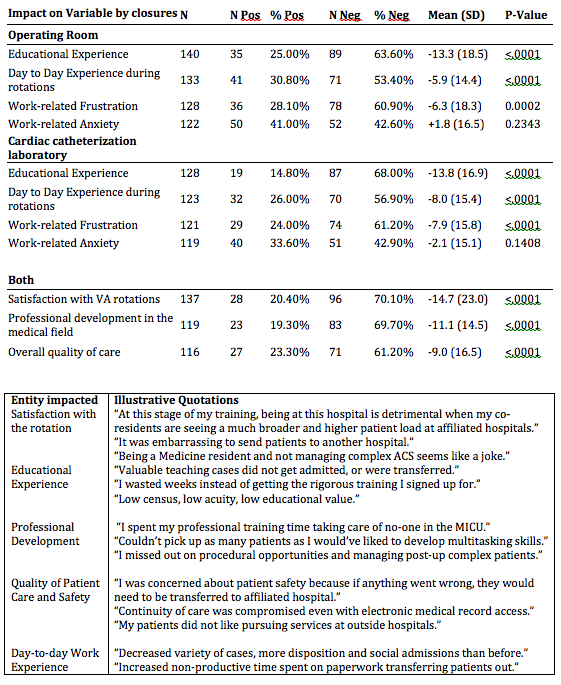
Results: Trainee Experience (Table 1): Of the 281 trainees who had worked at the affected site during closures, 172 (61.2%) responded to survey: 57% were PGY1-3, 54% were women, who spent mean of 5.7 weeks (SD=4.0) at the site. The most significant negative impacts related to education, professional development, satisfaction with rotations, and perceived quality of patient care (p<.001 for all). Trainees reported increased work-related frustration, with no impact noted on work-related anxiety. Negative impact was higher for PGY1-3 on professional development (p=0.012) and for students and PGY1-3 on their education (p=0.022). Inpatient workload and hospital quality measures (Figure 1): During the OR/CCL closures, daily bed occupancy was 40%-60%, as compared to 65-100% in 2017. Admissions/month during the closures declined by 12.3% (Surgery -23.4%, Medicine -10.3%, p<0.0001), with near-complete recovery in 2019. Total bed-days of care/month declined by 22.3% (Surgery -28.9% and Medicine -20.3%, p<0.0001). We found a significant decrease in inpatient workload for Medicine and medical subspecialties: they had 3,380 less patient encounters, a decrease of 38% overall compared to the same time period in 2017. This negative impact was felt across each specialty: a decline in workload by 8% for Gastroenterology, 14% for Hematology/Oncology, 28% for Hepatology, 31% for MICU, 33% for General Medicine, 42% for Renal, 50% for Cardiology, and 74% for Infectious Diseases.
Conclusions: We found that the unavailability of surgical and cardiac interventional services decreased the inpatient workload and inpatient census on not just surgical/interventional services, but also Internal Medicine and all Medicine subspecialties. Of notable interest, trainees of academic programs in Medicine and medical subspecialties reported that OR/CCL closures negatively impacted their education and professional development, as well as their perception of quality of patient care. This institutional experience provides opportunities for academic programs and hospitals to develop contingency plans for unanticipated interruption in services, as the impacts can be global, impacting services and affiliated academic training programs in unexpected, interdependent ways.