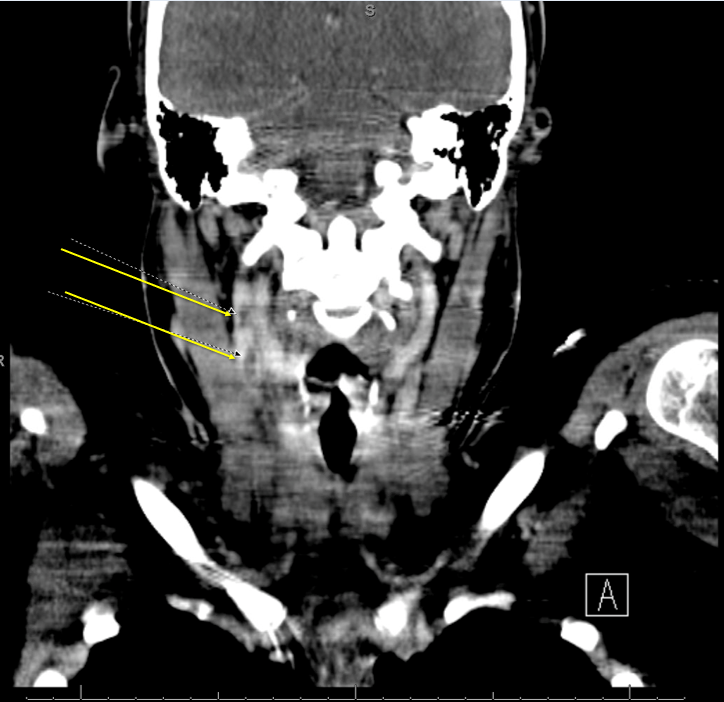
Case Presentation: A 20-year-old female with no past medical history presented to a rural hospital with shortness of breath, sepsis, and a several-day history of right-sided throat pain 2 weeks after a dental procedure. Chest x-ray demonstrated bilateral lung opacifications and blood cultures were positive for Streptococcus constellatus. She was started on broad-spectrum antibiotics and transferred to a larger center for workup of suspected acute infectious endocarditis. On physical exam, she appeared acutely ill. Labs showed leukocytosis, elevated lactate, metabolic acidosis, hyperbilirubinemia, anemia, severe thrombocytopenia, and elevated BNP. Transesophageal echocardiogram displayed no convincing evidence of endocarditis, but CT of the neck and chest with contrast revealed two foci of non-obstructive thrombi in the right internal jugular vein, and pulmonary nodules indicative of septic emboli. The patient’s presentation, findings, and her recent dental procedure were suggestive of Lemierre syndrome. She was started on apixaban and placed on IV ceftriaxone before later being discharged with a peripherally inserted central catheter for three-month long continued treatment.
Discussion: Jugular vein suppurative thrombophlebitis, also known as Lemierre syndrome, is defined by the presence of an infectious thrombotic embolus in the internal jugular vein. The source is typically pharyngitis, tonsillar infection, or more rarely, dental infections (<2%). Although it is rare (3 per million people), awareness is still critical since left untreated, it can be fatal.Lemierre syndrome is caused by bacteria invading through the carotid sheath in the parapharyngeal space resulting in an infectious internal jugular vein thrombosis. It commonly affects previously healthy patients in their twenties and thirties and is typically caused by Fusobacterium necrophorum. Rarely, other normal oral flora that may be introduced into the blood by oropharyngeal infections or dental procedures—gram-positive cocci in our case—may also occasionally be the culprit. In this patient, complications included septic emboli to the lungs, but other sequelae such as stroke and endocarditis have also been observed. Scientific advancements have significantly improved mortality rates from 32-90% in the pre-antibiotic era to 17% now. More recently, incidence rates have been rising likely due to the more conservative use of antibiotics to treat pharyngitis and tonsillitis.
Conclusions: Although most patients recover well with proper diagnosis and treatment, this disease can still be deadly. Practitioners should consider Lemierre syndrome in young patients who present with throat pain, sepsis, and suspicious findings on imaging.