Background: Burnout is a term used to describe an extended response to psychosocial and interpersonal stressors precipitated in a work-setting.1 Although there are many aspects of burnout, those commonly identified include increased emotional exhaustion, cynical attitudes towards others, and the tendency to view oneself negatively. Medicine is a common, and well-renowned field that is heavily impacted by emotional stress including burn out. This can not only have dire consequences on physicians’ health, but also negatively impact patient care and financially tax the healthcare system.2 Burnout rates have been found to range from 25% to 60% amongst all physicians. However, Internal Medicine residents, suffer from severe rates of burnout with up to 71% of residents affected by this.3 Given the COVID-19 pandemic, stress on medical providers is expected to increase due to multiple factors including increased work hours, docked raises, and emotional exhaustion related to patient care.
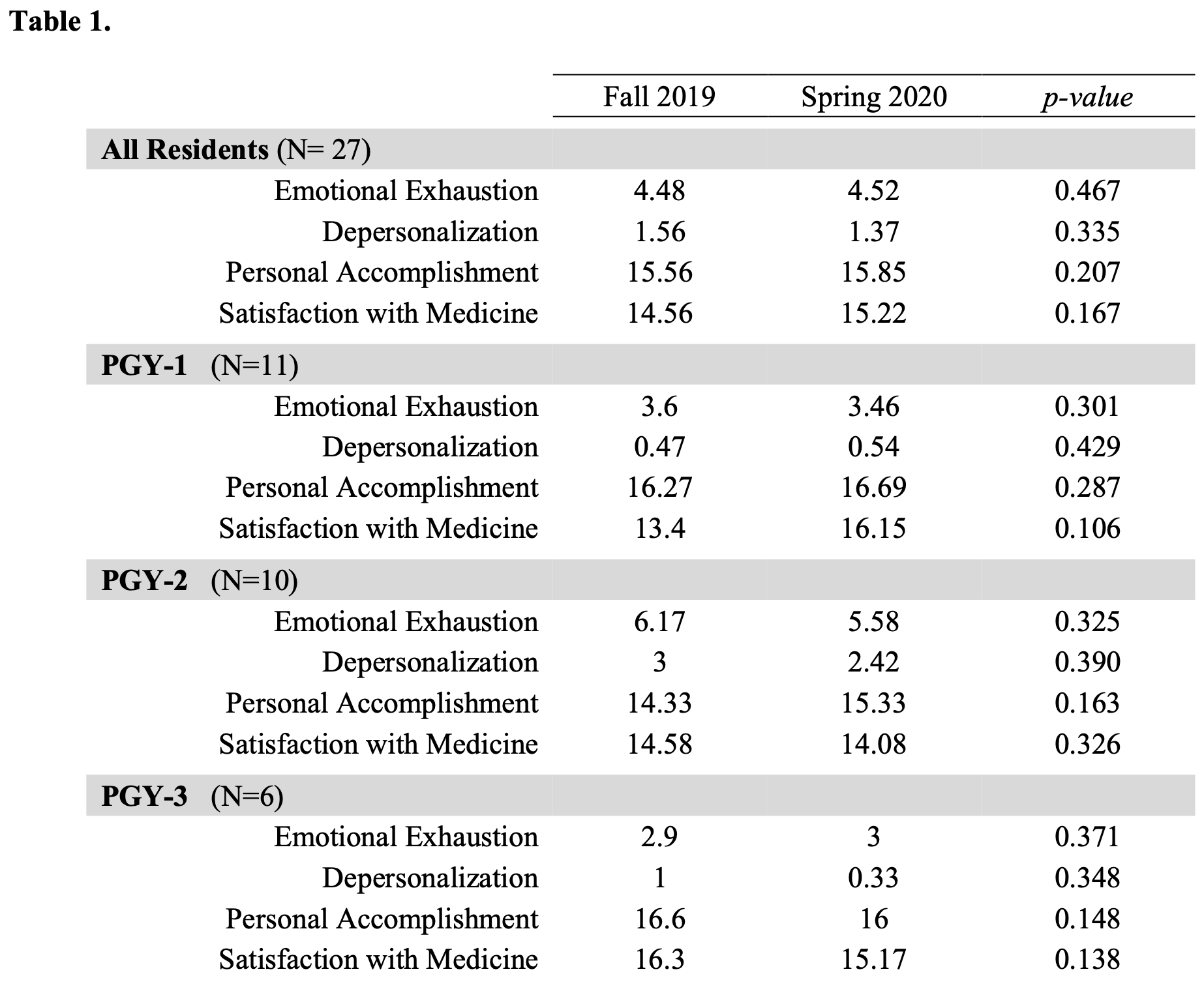
Methods: Abbreviated Maslach Burnout Inventory surveys were sent 6 months apart (October 2019 and April 2020) to a total of 50 residents at Geisinger Medical Center’s Internal Medicine Residency Program to evaluate burnout. Each survey contained 12 total questions for emotional exhaustion, depersonalization, personal accomplishment and satisfaction, that were answered on a linear scale from 0 to 6, with each category having maximum total of 18. Differences between the two groups were calculated using a paired sample T-test and a p-value below 0.05 was statistically significant.
Results: A total of 27 surveys from 6 months apart were received between first- (41%), second- (37%), and third-year residents (22%). Data was anonymized by program leadership and subsequently analyzed by the investigators. Comparison of the 6-month surveys showed no significant difference in any of the four categories, including emotional exhaustion (p-value = 0.487), depersonalization (p-value = 0.335), personal accomplishment (p-value = 0.207), and satisfaction with medicine (p-value = 0.167). No difference was noted when each class was analyzed individually.
Conclusions: This study revealed that COVID-19 did not impact resident burnout in a large rural academic hospital. One possible explanation of this finding includes protocols set forth by program leadership to stagger resident schedules to include “recovery time” synonymous with the classic week-on/week-off schedule of hospitalists. Additionally, residents were taken off elective rotations to decrease risk of exposure to the virus. However, some of the limitations of this study include its small sample size, and the decreased prevalence of COVID-19 patients compared to urban academic hospitals. Of note, a trend towards more burnout was noted amongst PGY-2 residents, however there is not enough data to clarify if this is individual specific, or a phenomenon that can be replicated in different residency programs.