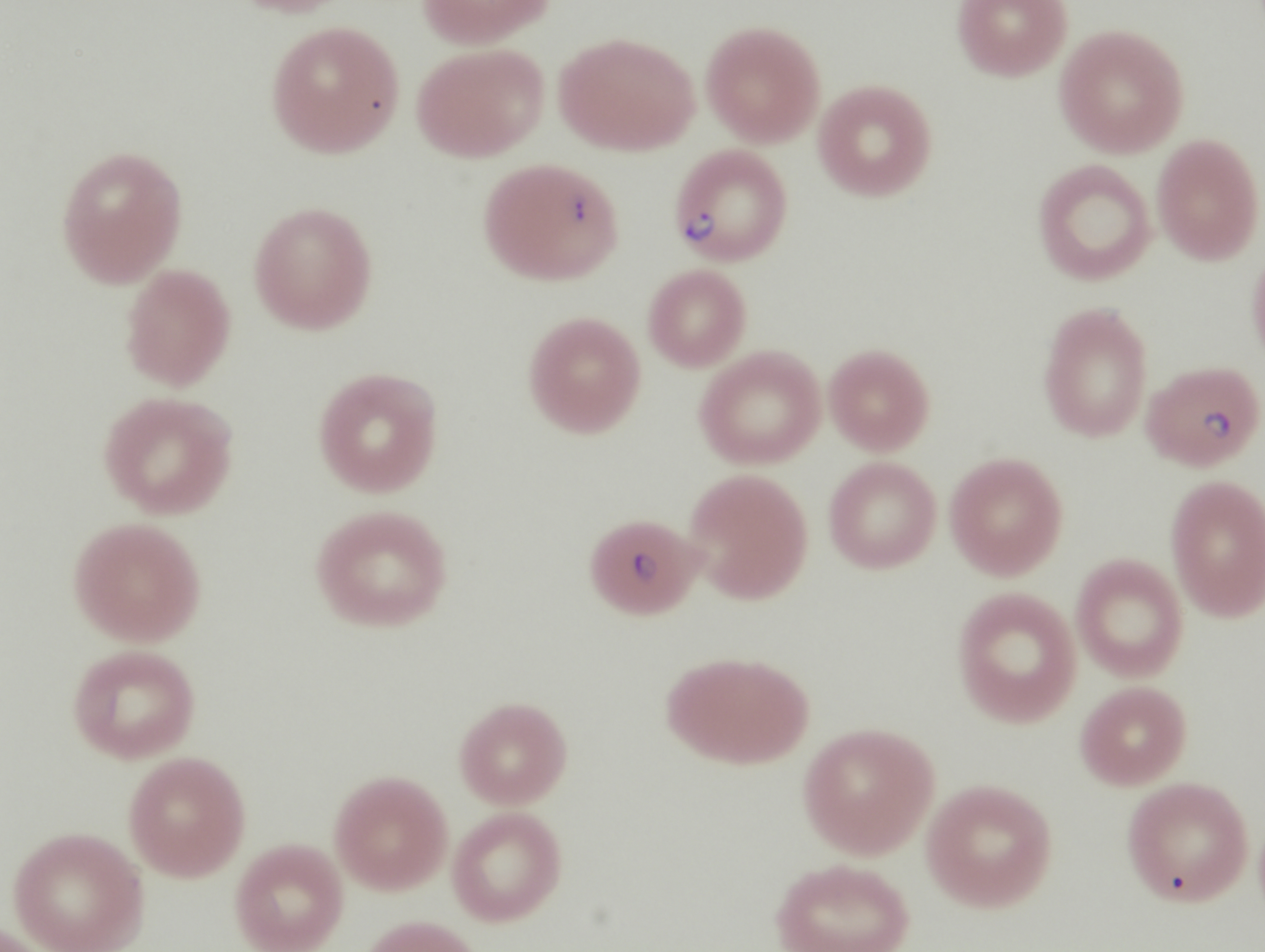
Case Presentation: A 60-year old male gardener presented with generalized body aches, night sweats, chills, malaise, fevers and headache (frontal and occipital) intermittently for a month. He reported abdominal pain, dyspnea, joint stiffness and myalgia. Around 2 weeks prior, the pain intensified and he received a treatment for upper respiratory infection with azithromycin. He finally presented to the ED with severe muscle aches, worsening headache (10/10), and high grade fevers (102-103F). He was given IV Doxycycline for Lyme (as his Lyme-Ab positive) and IV Ceftriaxone and admitted to the the floors. The patient denied nausea, vomiting or skin rash. He was ex-drinker and ex-smoker. He had a history of Lyme disease 2 years ago for which he was treated with Doxycycline. He also denied animal contact, tick bite or recent travel anywhere. On examination, Temperature 102.6F, Pulse 103/minute, Respiratory rate 22/minute, and BP 103/53 mmHg. The patient was awake and alert with positive painless scleral icterus and negative meningeal signs, jolt test, or focal deficit. Labs revealed pancytopenia (Hb: 8.3, TLC: 7.9, Plt: 34), electrolytes normal, elevated LFTs (AST: 139, ALT: 33, ALP: 185), bilirubin (Total: 10, direct: 7.5), PT: 12.7, INR: 1.3, and creatinine 1.27 mg/dL. CT abdomen with contrast showed thickening of gallbladder. Abdomen ultrasonography showed hepatospelenomegaly. The patient was fluid resuscitated, despite which he became unstable and transferred to the ICU for pressor support. Anaplasma co-infection was suspected based on rapidly declining hemoglobin and platelets. Babesia parasitemia level turned out to be 16% that reduced to only 9%. Azithromycin 500 mg daily, Atovaquone 750 mg daily, IV Ceftriaxone 1G twice daily, IV Clindamycin 600 mg 6 hourly and oral Quinine 650 mg tid. HIDA scan showed no concurrent cholecystitis. Diagnosis of severe Babesiosis with high level of parasitemia, hemolysis, splenomegaly, and septic shock was made. Patient was transferred to a tertiary center as patient began to have active hemolysis evidenced by elevated LDH, haptoglobin, and Schistocytes. He underwent two sessions of plasmapheresis for severe Lyme and Babesiosis. Antibiotics Clindamycin, Doxycycline, Quinine, and Ceftriaxone were continued for total of two weeks.
Discussion: Lyme disease (Borrelia burgdorferi) and Babesiosis (Babesia microti) are both tick-borne diseases, commonly encountered in Northeastern and Great Lakes regions of the United States. Co-infection with these two ticks is rare and underreported. It is important to recognize co-infection of these two conditions as it results in severe and prolonged disease manifestations. Sweeney et al., dos Stanose and Kain, and Adler et al. have reported this co-infection in 68 years old woman, a 59-year old man, and a 39-year old man, respectively. The severity of the condition is enhanced due to synergistic inflammatory response to both parasites.
Conclusions: Babesiosis coinfection with Lyme disease resulting in septic shock is rare. The percentage of co-infection with Babesia and Lyme disease is varied. Some studied have reported antibodies against both ticks in up to 66% cases.
.jpg)
