Background: Project Caring for Patients with Opioid Misuse through Evidence-Based Treatment (COMET) launched in 2019 to provide patients with opioid use disorders (OUD) individualized and evidence-based care at Duke University Hospital (DUH). Patients with OUD have higher rates of self-directed discharge (SDD) which is associated with higher healthcare utilization costs, hospital readmissions, and adverse health outcomes [1-4]. We identified clinical and sociocultural drivers of SDD in patients with OUD as a basis for future interventions to reduce SDD in this group at DUH. Prior studies have identified reasons for SDD from patient interviews, but to our knowledge, this is the first to look at documented patient-provided reasons for SDD in this population through chart review.
Methods: A PubMed search was conducted for articles on SDD, of which 14 were selected. Characteristics found to be associated with SDD in patients with substance use disorders were included as categories to inform our chart review. A convenience sample of 30 charts for patients who received a COMET consult for OUD and had an SDD between December 2019 and October 2022 was reviewed to identify patient characteristics and patient-provided reasons for SDD.
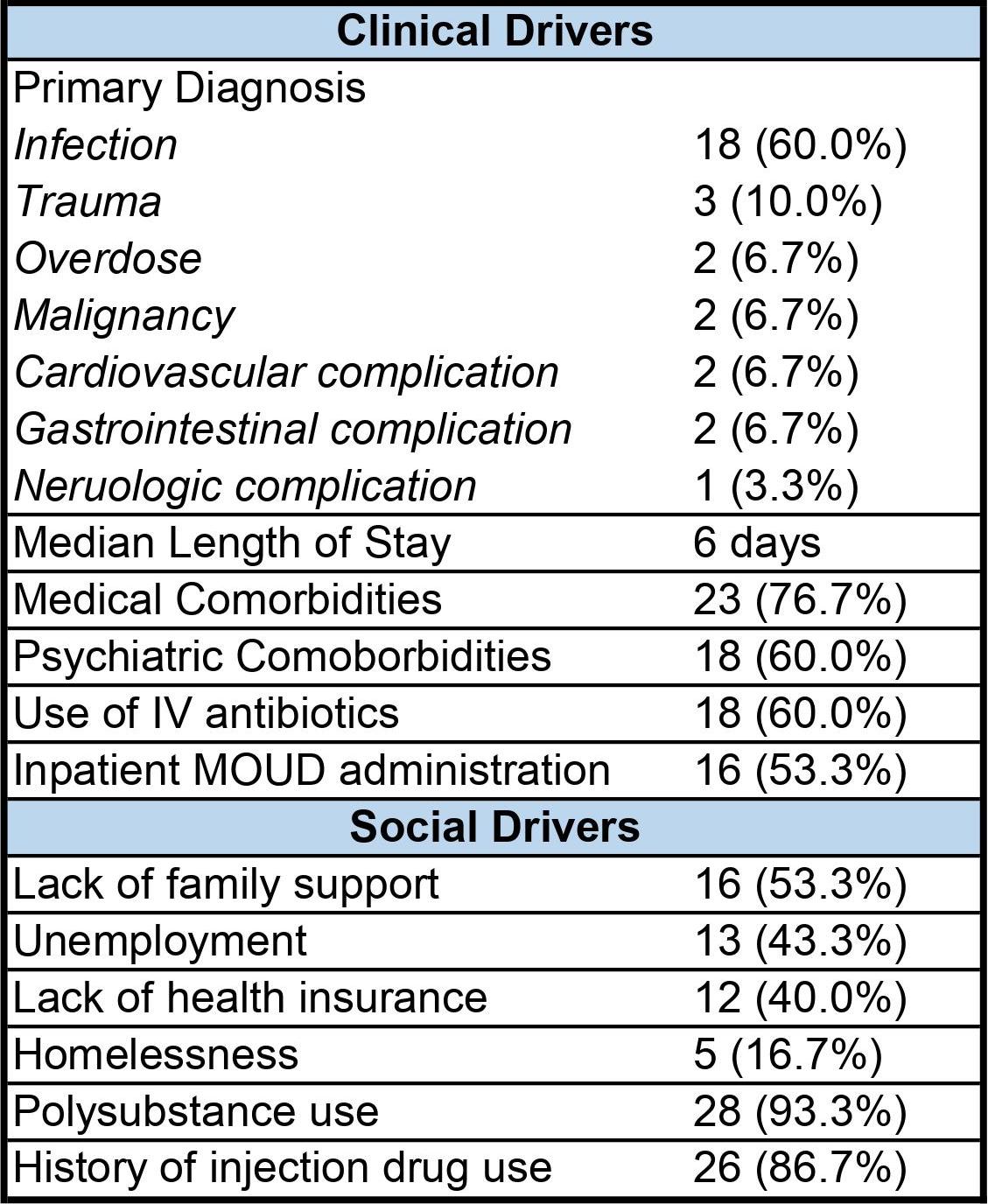
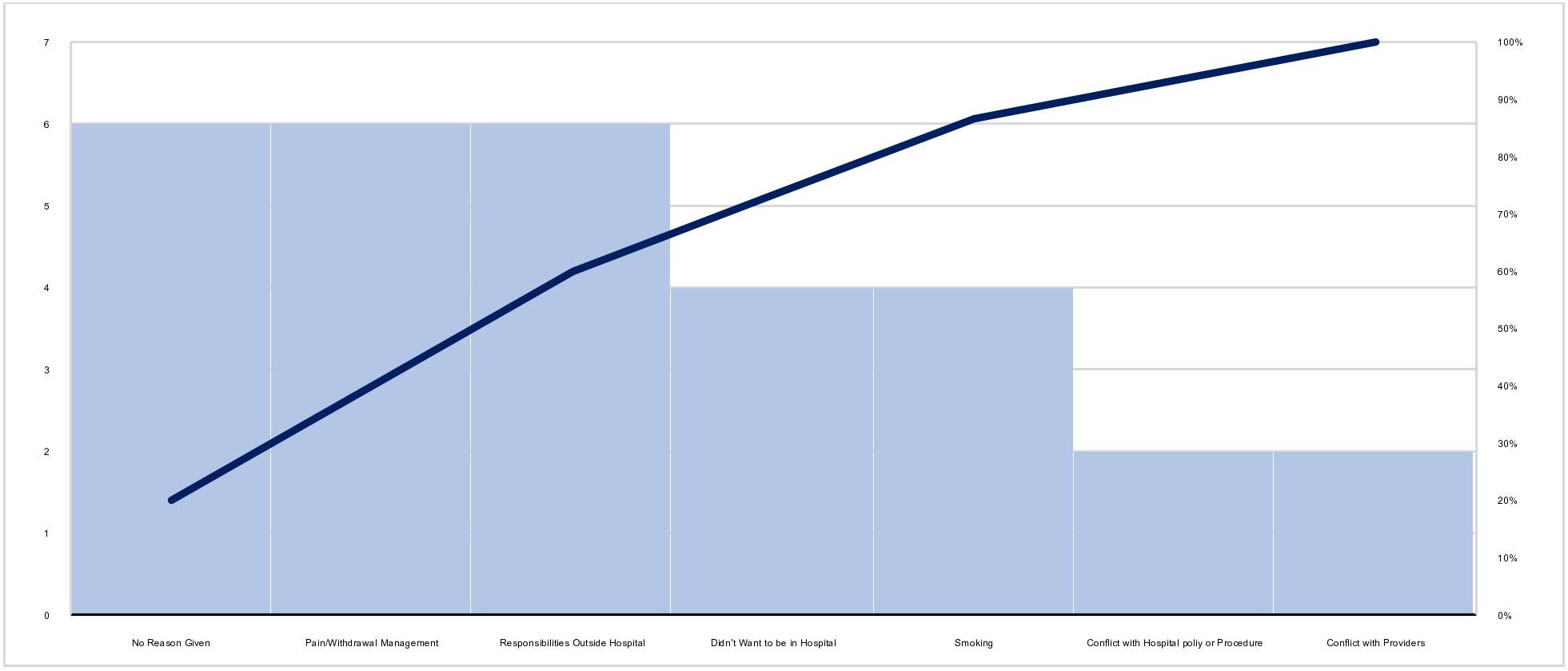
Results: Of the 30 patients reviewed, median age was 39.5 years. Thirty percent were Black, 3.3% were Hispanic, and 6.7% did not report their race. Most patients (76.7%) had preexisting medical comorbidities and 60.0% had psychiatric comorbidities. Sixty percent had a primary diagnosis of infection and 10.0% had a primary diagnosis of trauma. Approximately half (53.3%) of patients were given medications for OUD (MOUD) while inpatient. The median length of hospital stay was 6 days. Most (93.3%) patients reported polysubstance use and 86.7% reported injection drug use. Approximately half (53.3%) of patients had no familial support, 43.3% were unemployed, 40.0% had no health insurance, and 16.7% were unhoused. Patient-provided reasons for SDD included inadequate pain and withdrawal management (20.0%), responsibilities outside the hospital (20.0%), desire to smoke (13.3%), wanting to leave the hospital (13.3%), and conflict with hospital policy (6.7%) and providers (6.7%). Twenty percent of patients had no listed reason for SDD.
Conclusions: Patients with OUD who self-direct their discharge have high rates of medical and psychiatric comorbidities. Most patients were admitted for infection and had a history of injection drug use, highlighting the importance of harm reduction education as part of a comprehensive treatment plan. Patients with OUD and SDD face significant social barriers to care that are important to address while hospitalized. Given the significant proportion of patients who did not get MOUD and reported inadequate pain and withdrawal management as a reason for SDD, protocols for early and low barrier MOUD access should be prioritized. High rates of SDD associated with a desire to smoke suggest a need for greater nicotine replacement therapy efforts or a consideration for hospital policy changes to permit smoking. The significant portion of patients with SDD without a provided reason suggests the importance of open conversations about discharge during a patient’s stay. Further research with a larger sample size could better illuminate trends in SDD for patients with OUD. By identifying salient features of SDD in this population, hospitals and providers can tailor interventions to their patients with the aim of reducing rates of SDD through better informed and higher quality care.