Case Presentation: A 28-year-old female with unremarkable past medical history presented with a 3-day history of fever, diffuse abdominal pain, nausea, and vomiting.
Vital signs were significant for temperature of 38.3 C and heart rate of 180 BPM. Physical exam revealed left-sided costovertebral angle tenderness.
Laboratory studies were notable for total bilirubin 2.7 mg/dL, direct bilirubin 1.8 mg/dL, lactate 2.4 mmol/L, thyroid stimulating hormone less than 0.007 UIU/mL (undetectable), free thyroxine (FT4) more than 8 ng/dL (above detectable limit), thyroid stimulating immunoglobulin more than 500% (above detectable limit), normal urine drug screen, large leukocyte esterase on urinalysis, and urine culture with pan-sensitive E. coli.
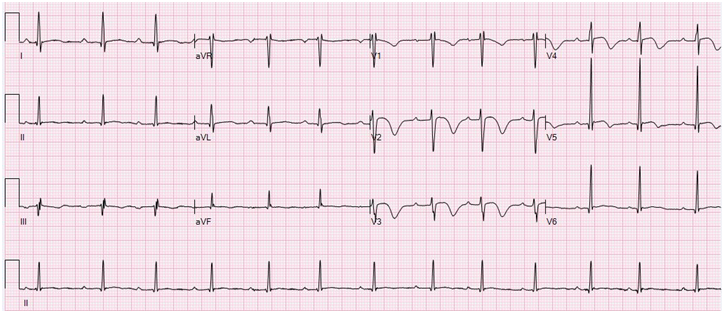
The electrocardiogram (ECG) at the time revealed sinus tachycardia at 145 BPM but otherwise without abnormality.
CT abdomen and pelvis with contrast showed wedge-like regions of hypoattenuation within the left renal cortex of kidney, and small region of mass-like hypoattenuation within the right cortex of kidney consistent with bilateral pyelonephritis.
The patient was given 5 mg of intravenous metoprolol for tachycardia and admitted for thyroid storm and urosepsis. She was treated with propylthiouracil (PTU), propranolol, saturated solution potassium iodide (SSKI), hydrocortisone, and cholestyramine.
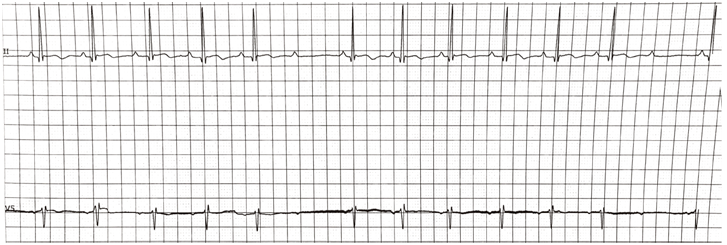
The patient’s tachycardia resolved on hospitalization day 2. On hospitalization day 3, the patient developed first degree AV block (Figure 1) then progressed to intermittent second degree Mobitz type 1 AV block (Figure 2) 8 hours after missing a dose of propranolol, which was resumed, an additional dose of IV hydrocortisone was given and the AV block resolved on day 4 of hospitalization.
After the atrioventricular block resolved, transthoracic echocardiogram revealed an ejection fraction (EF) of 62% without structural or functional abnormality. The patient was then discharged with methimazole, propranolol to follow up in clinic for Grave’s disease in 4 weeks with improved FT4 at 1.7.
Discussion: Second or third degree AV block associated with hyperthyroidism is very rare, and it has been reported in association with acute infectious or inflammatory state, hypercalcemia, digitalis, or concomitant heart disease. In this case, absence of pre-existing conduction delay at presentation and the staged resolution of AV block following a reduction in thyroid hormone levels while on propranolol implicated high circulating thyroid hormone and/or TSI levels as the cause for her AV block. Optimal therapy for AV blocks associated with thyroid storm is not established although therapy consists of antithyroid medication was successful in two cases. Several cases raised concern for beta-blockers’ effect in progression of AV block in hyperthyroidism, and advised cautious use of beta-blockers in such condition. However, there is no documented beta-blockers’ use in AV blocks associated with thyroid storm. The development of first degree AV block in thyroid storm when a dose of propranolol was not administered, its progression to second degree AV block as time elapsed, and its gradual resolution with resumption of propranolol appear to contradict the predominant opinion on beta-blockers’ use in such condition and may suggest a different mechanism as the current literature on AV blocks in thyroid storm is scarce.
Conclusions: Optimal therapy for AV blocks in thyroid storm is not established although antithyroid medication was successful in two cases and in this case.