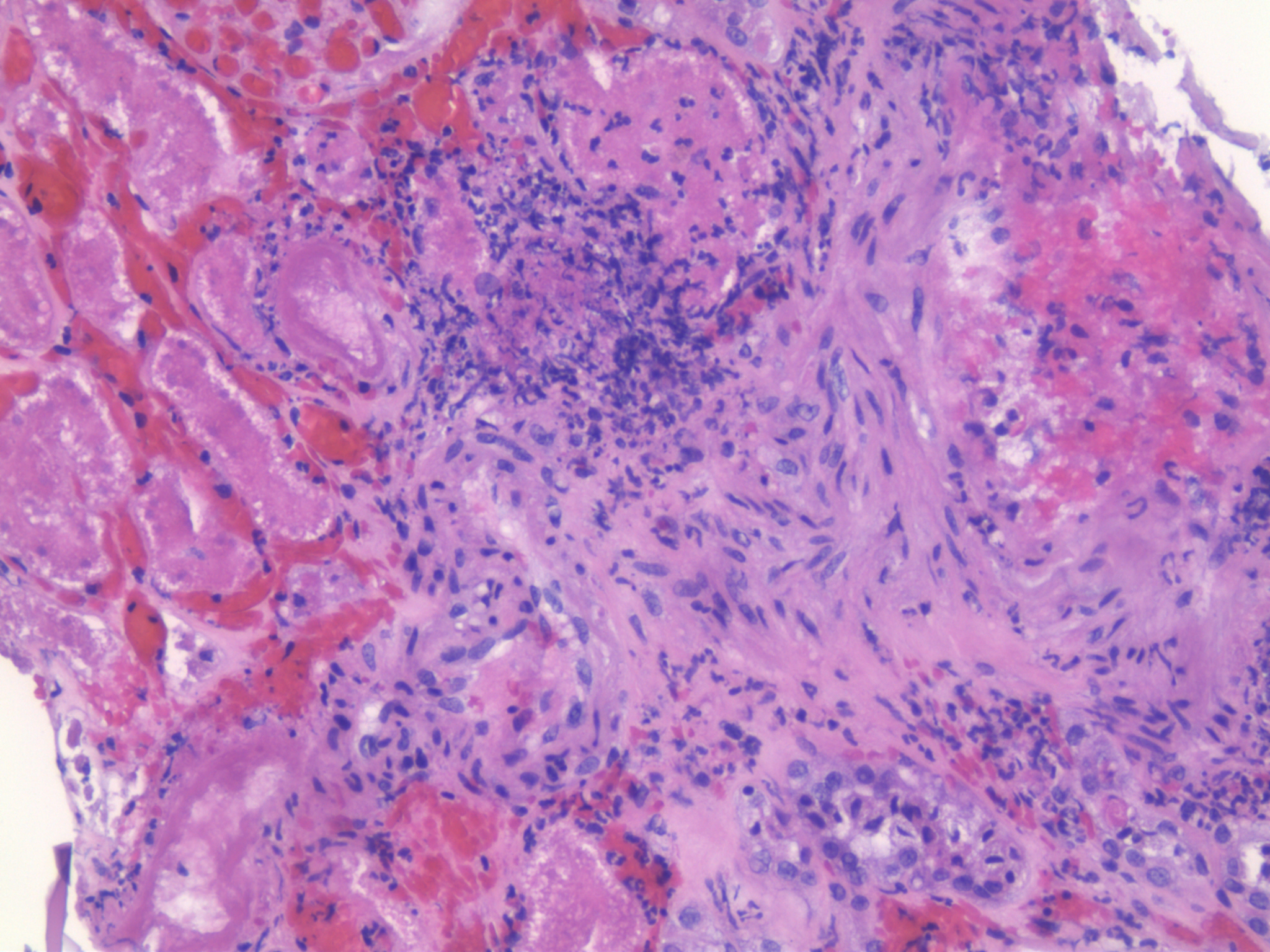
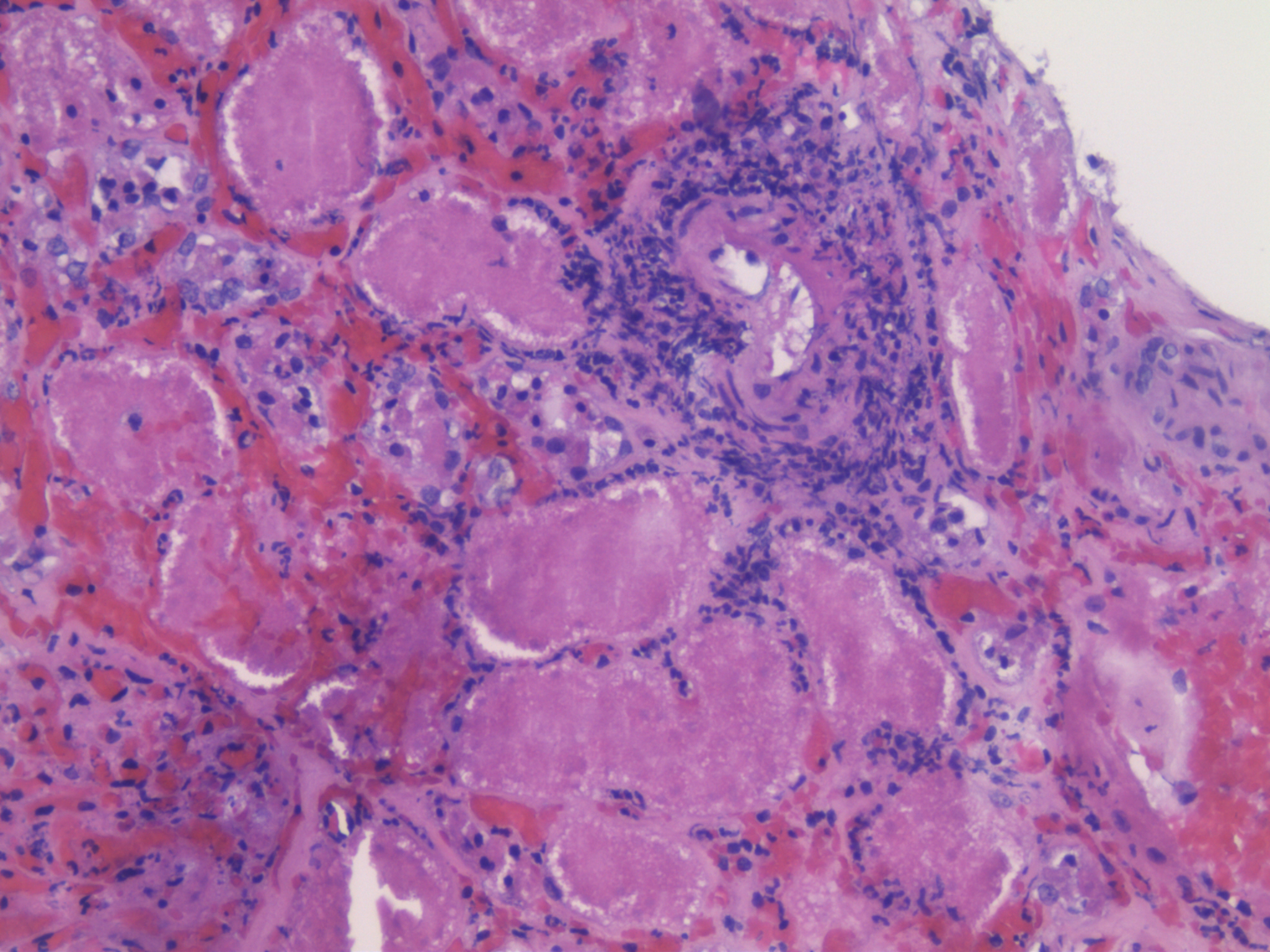
Case Presentation: A 53-year-old male with a history of Goodpasture syndrome, systemic lupus, and Wegener’s granulomatosis underwent a deceased donor kidney transplant for end-stage renal disease. Two days post-surgery, the patient developed anemia and thrombocytopenia, elevated lactate dehydrogenase, and increased creatinine, prompting a preemptive diagnosis of TTP. Plasmapheresis was initiated every other day, alternating with hemodialysis, and Tacrolimus was discontinued due to concern for medication-induced TTP. After several sessions of plasma exchange, lactate dehydrogenase levels decreased significantly while the creatinine remained elevated. Platelet count stabilized, and hemoglobin levels reached a nadir of 8.4 g/dL. An ultrasound was performed, revealing no flow in the superior pole of the right lower quadrant transplanted kidney, and an allograft biopsy showed extensive parenchymal ischemic necrosis, arterial and capillary thrombi, and evidence of ischemic necrosis of the tissue. ADAMTS 13 levels returned as unmeasurable, < 5, consistent with the microangiopathic process, and patient underwent nephrectomy due to poor perfusion of the allograft transplant.
Discussion: TTP, occurring post kidney transplant, is a critical hematological complication that significantly impacts graft and patient outcomes. The diagnosis was made by a combination of low platelet count, anemia, reduced haptoglobin, elevated LDH, and the presence of schistocytes on the blood smear. The cause of TTP development in this case is most likely multifactorial. One possible scenario is that the patient might have donor-derived TTP, which contributed to the overt manifestation of thrombotic microangiopathy, leading to poor graft function. To address the issue, the patient underwent nephrectomy, which improved her overall condition. The drug Tacrolimus, used in transplant services, has also been associated with thrombotic microangiopathy by inducing endothelin secretion and exacerbating the hemolytic process. ADAMTS 13, a key factor which cleaves von Willebrand factor, and its deficiency leads to large vWF multimers binding to platelets forming microthrombi. Plasma exchange is the best initial treatment as it replaces the missing ADAMTS13 and removes inhibitors. Post transplant thrombotic microangiopathy has a poor prognosis with a high mortality rate and significant graft loss within the first two years after diagnosis.
Conclusions: This case demonstrates the importance of attentiveness and alertness in patients who develops TTP in the setting of kidney transplant as it can happen super early post-transplant. It serves as an alert to clinicians for timely detection, diagnosis, and initiation of treatment to prevent mortality.