Background: Delays in antibiotic administration in sepsis – particularly after the development of hypotension – are associated with increased mortality. Current guidelines recommend antibiotic initiation within one hour of sepsis recognition. However, it is not known how timing of hypotension relates to the timing of meeting sepsis diagnostic criteria and the initiation of treatment. We aimed to determine how high-risk septic adults presenting to the Emergency Department (ED) who develop hypotension differ in their time to meeting sepsis criteria and antibiotic initiation.
Methods: We extracted data from the electronic health record (EHR) on all adults presenting to a single academic ED between 6/1/2012 and 12/31/16 with suspected infection (blood cultures drawn, intravenous antibiotics within 48 hours) and validated EHR sepsis surveillance criteria (change from baseline Sequential Organ Failure Assessment Score (SOFA) of at least 2 by 48 hours and at least 4 antibiotic days unless death or discharge to hospice sooner; or validated sepsis discharge code) who developed hypotension (SBP <90) within 72 hours of presentation. Timestamped EHR-derived measurement to systemic inflammatory response syndrome (SIRS) and SOFA score of at least 2 and SBP<90 were used to assess recognition of sepsis and hypotension. We categorized patients by time from hypotension until antibiotic administration: 1. Antibiotics before hypotension; 2. Antibiotics 0-60 minutes after hypotension; 3. Antibiotics >60 minutes after hypotension.
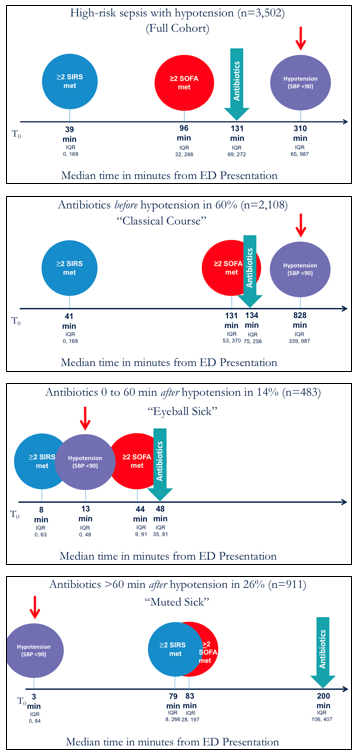
Results: Among 3,502 patients with sepsis who developed hypotension within the first 72 hours of presentation, antibiotic administration categories identified discrete presentations of sepsis (Figure). While 60% (N=2,108) receiving antibiotics before hypotension followed a “classical course”, meeting SIRS and SOFA criteria many hours before hypotension, both the “eyeball sick” cohort (n=483, 14%) who received antibiotics within 60 minutes of 1st hypotension and the “muted sick” cohort (n=911, 26%) who received antibiotics >60 minutes after hypotension developed hypotension soon after ED triage. While the “eyeball sick” group also met SIRS and SOFA criteria soon after ED triage, the “muted sick” group had a comparative lag in meeting SIRS and SOFA. Even after meeting full sepsis criteria, antibiotics were not administered for 2 additional hours and 3.3 hours after first hypotension (Figure).
Conclusions: Among septic patients with hypotension, we identified three discrete subtypes of patients according to timing of antibiotics from the onset of hypotension. Our findings suggest a heterogeneous disease trajectory of hypotensive patients with sepsis. Most notably, 26% were categorized into the “muted sick” subset of patients who develop hypotension soon after triage, but have later development of SIRS and SOFA criteria and much later receipt of antibiotics. Early hypotension may be the “canary in the coal mine” for these high-risk patients and thus warrant modification of current sepsis alert systems to avoid delayed sepsis recognition and antibiotic administration.