Background: Handoff is defined as the transfer of information and accountability between providers. In hospital medicine, handoffs occur between day, swing and night providers, risking gaps in communication that can lead to errors and uncertainty in management. Communication deficiencies are identified as a root cause in 70% of sentinel safety events. Optimal implementation of structured handoff on a direct-care hospitalist service is not well described.We hypothesized that the implementation of a standardized IPASS-based daily handoff embedded within our electronic medical record (EMR) would improve hospitalist satisfaction with the handoff process, reduce perceived time spent on handoff and maintain perceived handoff safety.
Methods: At our 600 bed, tertiary care urban teaching hospital, daily handoff within the 90-person hospitalist group was historically performed using a semi-structured free-text email exchanged by day, swing and night providers. A standardized handoff tool using IPASS structure was developed using available fields in our EMR. These included Illness Severity, Patient Summary, Action List/To-Dos and Situational Awareness/Contingencies as well as space to record cross-cover events. A user guide was developed by a volunteer task force of hospitalists using an iterative process until consensus was reached. The new handoff process was introduced to hospitalists through email and faculty meetings. On-site support was available for troubleshooting during roll-out.A survey was sent to daytime and cross-cover (swing and night) hospitalists to assess satisfaction, perception of time spent on preparing handoff, and perceived safety of the handoff process prior to the implementation of the EMR-based handoff and again four months after implementation.
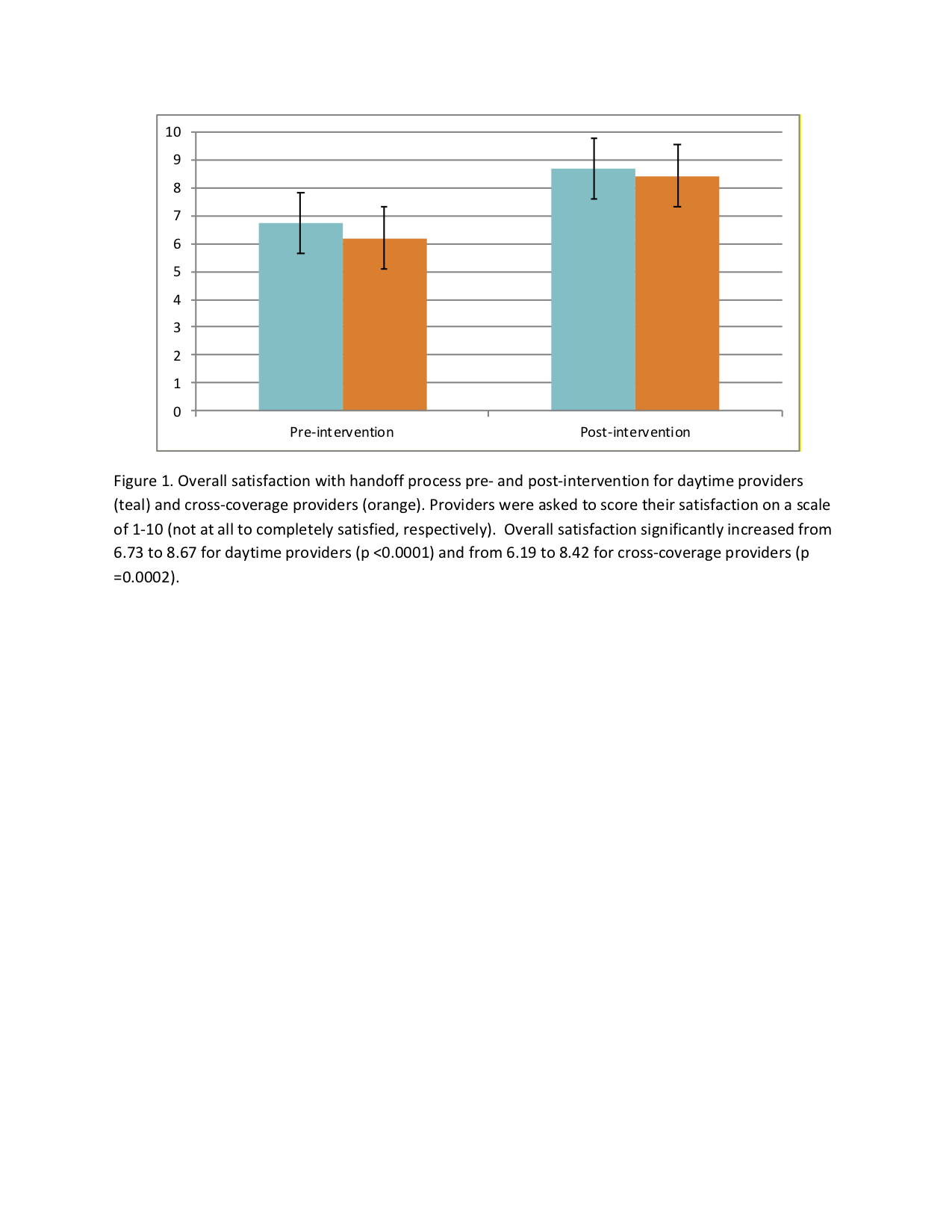
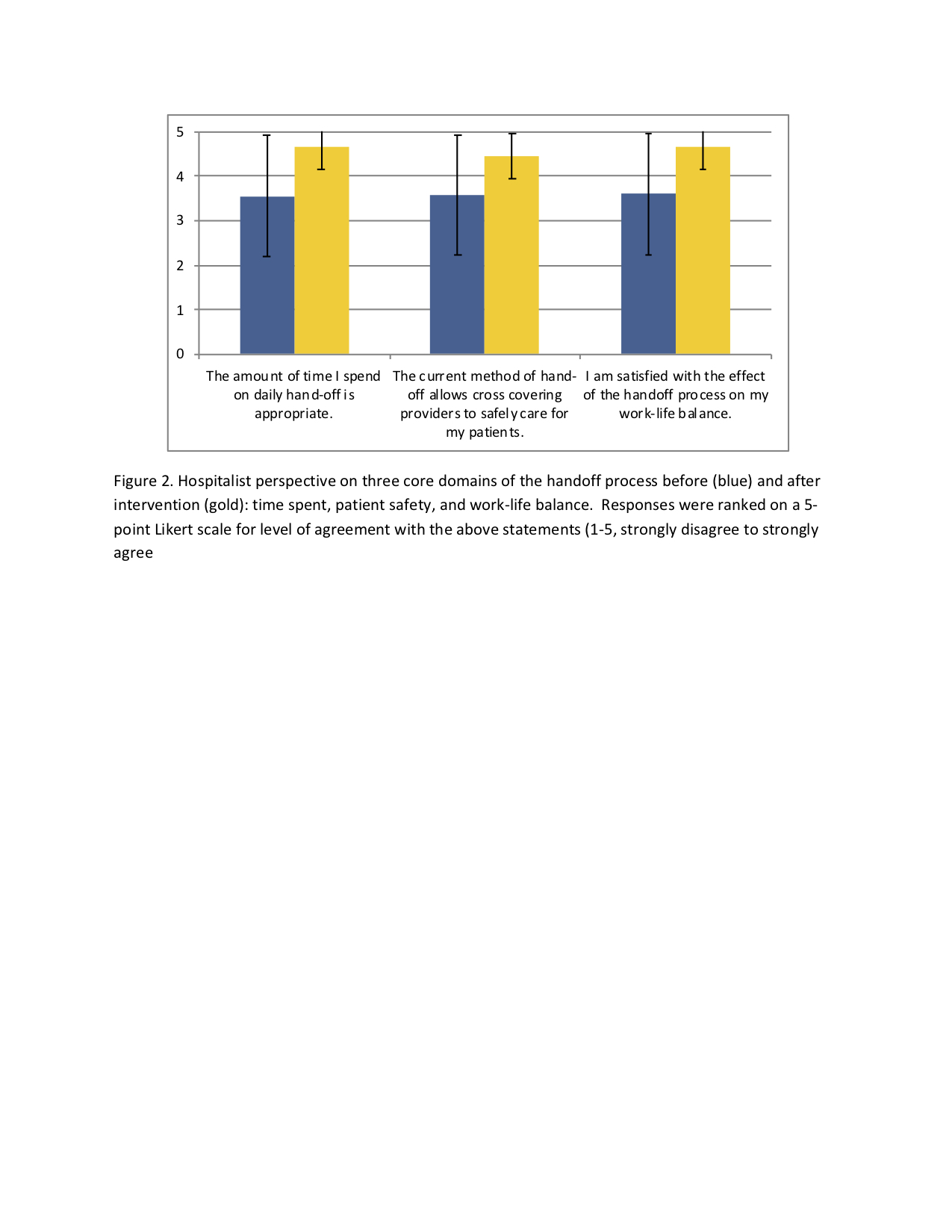
Results: Of the 90-person hospitalist group, 72 worked relevant shifts during the study period and 100% implemented the change during the first shift worked after roll-out. Response rates were 57% (41/72) to the first survey and 56% (40/72) to the second survey. Survey results were analyzed using unpaired t-tests.Average satisfaction with daily handoff as rated from 1 (completely dissatisfied) to 10 (completely satisfied) increased significantly from 6.73 to 8.67 (P<0.0001) (Fig 1). Time spent by the day hospitalist in preparing handoff decreased from 22 minutes to 16 minutes daily (p=0.02). There were also statistically significant improvements in hospitalists’ reported perceptions of efficiency, safety, and work-life balance (Fig 2). These improvements were reported by both day and cross-cover providers.
Conclusions: In this intervention, we aimed to assess the impact of a transition from free-text, email-based handoff to a standardized, IPASS structured, EMR-based handoff tool. The transition led to a statistically significant improvement in hospitalist satisfaction with daily handoff overall and a reduction in time spent preparing handoff. In addition, there were significant improvement in hospitalists’ perceptions of efficiency, the ability to promote safe cross-cover care, and work-life balance. Hospitalist groups could consider similar interventions to improve providers’ experience with these daily care transitions.