Background: Prevalence of burnout is significantly higher in physicians than general population. Burnout is expected to result in decreased personal well-being, however, relationship between physician burnout and well-being is unexplored. Therefore, our aim was to examine the relationship between burnout and well-being among medical staff physicians of an academic hospital.
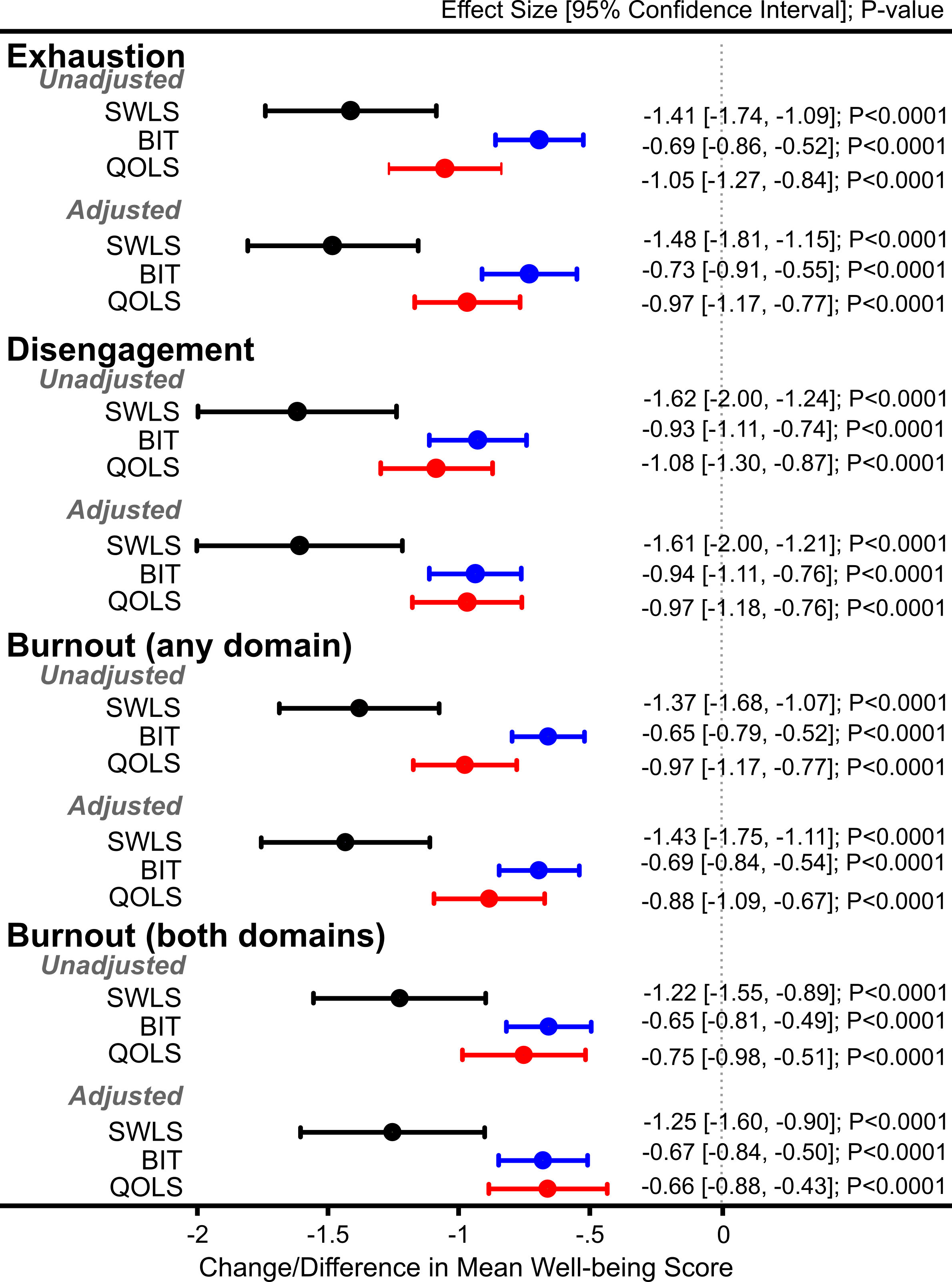
Methods: All medical staff physicians and residents were asked to complete an electronic survey via email. The survey contained demographic questions, a burnout questionnaire (Oldenburg Burnout Inventory [OBI]) and three well-being questionnaires; a cognitive measure of satisfaction with life (Satisfaction With Life Scale [SWLS]), a measure of psychological well-being (Brief Inventory of Thriving [BIT]), and a measure of overall personal well-being (Quality of Life Scale [QOLS] by Flanagan). OBI measures burnout using two domains, exhaustion and disengagement while SWLS, BIT, and QOLS measure well-being along one scale. Questionnaires were scored as recommended by their authors and mean scores were generated for each. Overall burnout was defined using two variables; one, when burnout was present on both exhaustion (mean score>2.25) and disengagement (mean score>2.10) scales (burnout on both domains [BBD]) and second when burnout was present on either of the two domains (burnout on any domain [BAD]). We used linear regression with bootstrap method to determine the relationship between the three measures of well-being and individual burnout domains and the two overall burnout variables (BBD and BAD) without and with adjustment for age, race, gender, and faculty or resident status.
Results: Of the 228 out of 685 physicians who completed survey (response rate=33%), 157(69%) were faculty, 78 (34%) were females, and 180 (80%) were Caucasians. Mean(SD) age was 42(13) years, exhaustion 2.5(0.48), disengagement 2.2(0.43), SWLS 4.9(1.3), BIT 4.2(0.67), and QOLS 5.2(0.95). Exhaustion was >2.25 in 144 (64%) physicians, disengagement was >2.10 in 137 (61%), BBD was present in 106 (47%), and BAD in 175 (77%) physicians. Exhaustion, disengagement, BBD, and BAD were strong predictors of low scores on SWLS, BIT, and QOLS in unadjusted and unadjusted models (Figure).
Conclusions: Physician burnout is a strong predictor of poor satisfaction with life, psychological well-being, and quality of life. System-level interventions combating burnout may help to promoting well-being among physicians.