Background: Black seniors have historically had higher readmission rates than white seniors, and hospitals that treat more black seniors have been disproportionately penalized the Medicare Hospital Readmissions Reduction Program (HRRP). Consequently, the policy could exacerbate racial disparities. We sought to determine whether, under the HRRP, trends in 30-day post-discharge mortality differed between black and white seniors.
Methods: In an interrupted time-series analysis, we used linear regression models to estimate risk-adjusted observed mortality rates and risk-adjusted projected rates based on population-specific pre-HRRP trends. We then compared observed and projected rates within each racial group (∆) after HRRP implementation, and trends between racial groups (∆∆).
Study hospitals were eligible for the HRRP in fiscal years 2013 and 2014, as per the Medicare HRRP payment adjustment dataset. Subjects included black and white Medicare fee-for-service beneficiaries age 65 or older with an index discharge from a study hospital that occurred between January 1, 2007 through November 30, 2014 and a principal diagnosis of AMI, HF, or pneumonia based on ICD-9-CM codes used under the policy. The unit of analysis was an eligible index hospitalization and subsequent 30-day post-discharge period, as per the HRRP. Exposures were hospital discharge during pre-HRRP (1/2007 to 3/2010), anticipation (4/2010 to 9/2012), and HRRP penalty (10/2012 to 12/2014) periods. The main outcome was 30-day post-discharge all-cause mortality.
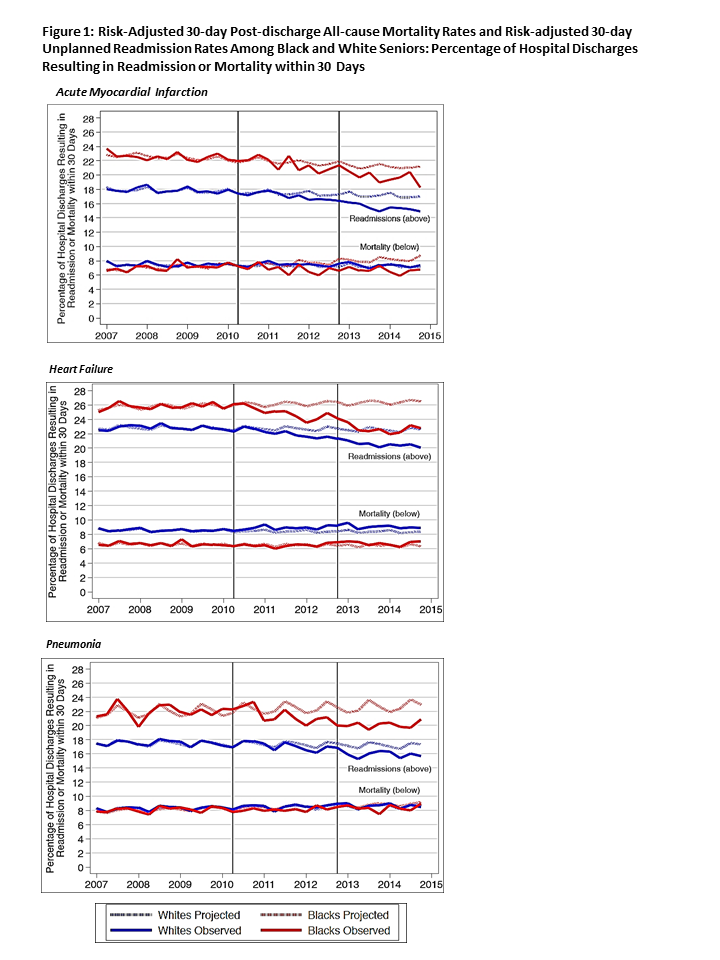
Results: Black seniors had 627,373 index discharges (9.7%) while white seniors had 5,845,130 (90.3%). For AMI, HF, and pneumonia, respectively, pre-HRRP mortality rates were 7.04%, 6.69%, and 8.08% among black seniors and 7.47%, 8.56%, and 8.27% among white seniors.
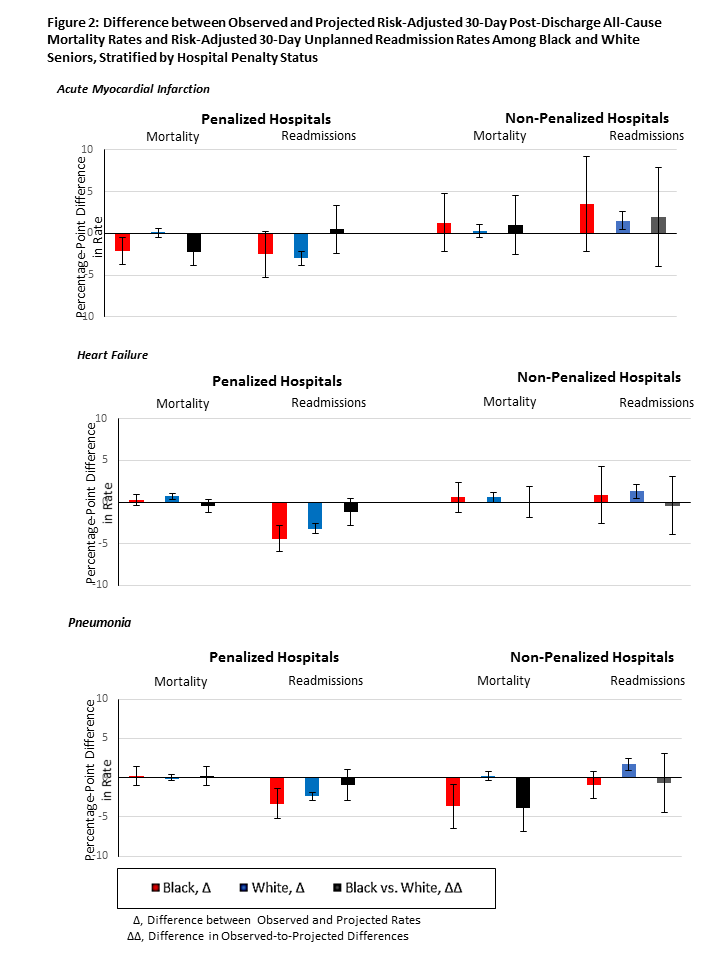
By the HRRP penalty period, observed mortality for AMI declined more, relative to projections based on pre-HRRP trends, among black than white seniors (∆∆ -1.65 percentage points, 95% CI -3.19 to -0.10, P=0.037). For HF, mortality rose relative to projections among white seniors but not among black seniors; however; mortality trends did not differ significantly between black and white seniors (∆∆ -0.37 percentage points, 95% CI -1.08 to 0.34, P=0.305). For pneumonia, observed mortality was similar to projections in both racial groups, and mortality trends did not differ by race (∆∆ -0.54 percentage points, 95% CI -1.66 to 0.59, P=0.352). Changes in mortality trends were similar or more favorable among black seniors relative to white seniors at both penalized and non-penalized hospitals.
Conclusions: Under the HRRP, racial disparities in short-term outcomes remained stable or improved. These findings provide reassurance that certain value-based payment policies can be implemented without exacerbating racial disparities.