Background: The first Multicenter Medication Reconciliation Quality Improvement Study (MARQUIS1) demonstrated that implementation of a medication reconciliation best practices toolkit decreased total unintentional medication discrepancies in 5 hospitals. Incorporating lessons learned from MARQUIS1, we implemented a refined version of the toolkit in a larger, more diverse sample of hospitals.
Methods: Eighteen sites were selected via a formal application and review process to implement the revised toolkit. This quality improvement (QI) project offered 17 intervention components. One of 8 hospitalists trained in physician-mentored QI coached each site via monthly calls and 1-2 site visits over the 18-month intervention period. Each site’s QI team assessed local policies and practices, identified improvement opportunities, and implemented one or more toolkit components. The primary outcome was unintentional medication discrepancies in admission or discharge orders, measured by comparing admission/discharge orders to a gold standard medication history taken by trained study pharmacists, using medical record review to determine whether discrepancies were unintentional. We used interrupted time-series (ITS) analysis to determine the effects of the intervention over time, adjusting for baseline temporal trends. We modeled the number of discrepancies per patient using multivariable Poisson regression adjusted for patient covariates, with total number of medications as a model offset, and clustered by site. We also conducted on-treatment analyses to determine the effects of a patient receiving at least one intervention, e.g., having a best-possible medication history taken by trained personnel.
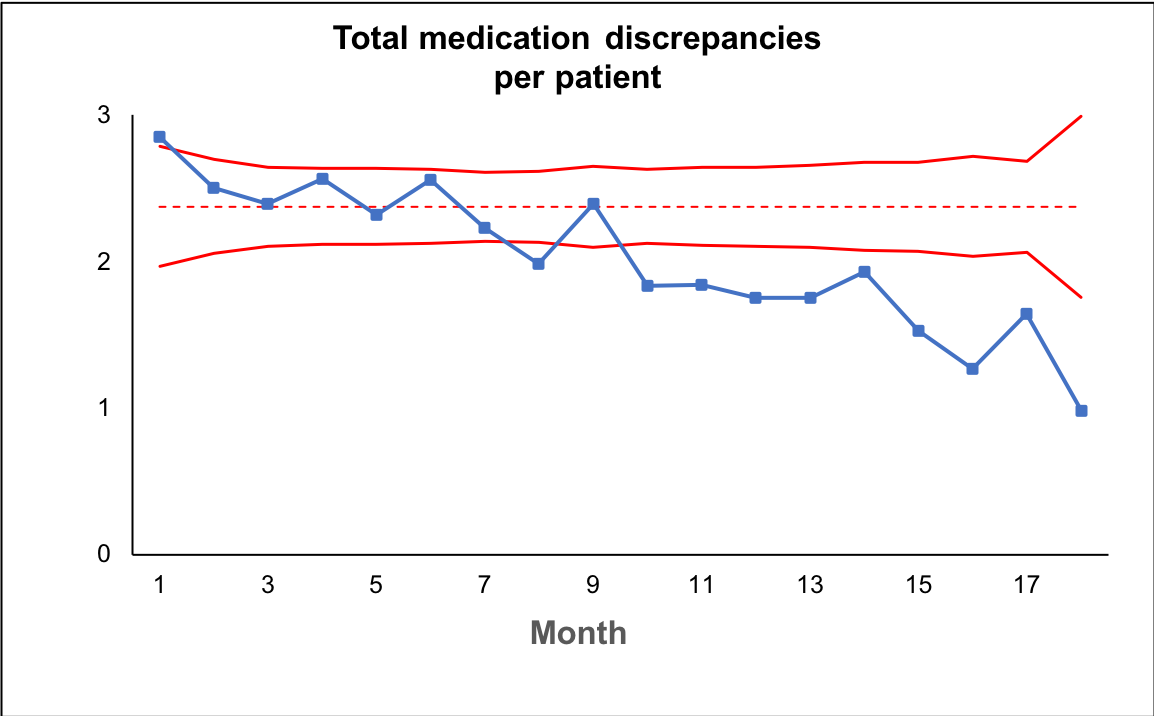
Results: All 18 sites implemented 1 to 15 toolkit components. One site did not collect enough data to be included in these analyses. Of the remaining 17 sites, there were 1229 patients in the pre-intervention period and 3718 in the post-intervention period. During the intervention, sites saw a steady decline in their medication discrepancy rate from approximately 3 discrepancies/patient to 1 discrepancy/patient (Figure 1). In ITS analysis, sites saw a 5% relative decrease in discrepancies per month over baseline temporal trends (adjusted incidence rate ratio 0.95 (95% CI 0.93-0.97), p<0.001). Patients who received at least one patient-level intervention had 53% fewer discrepancies than those who did not receive any (adjusted IRR 0.47 (0.45-0.49), p<0.001).
Conclusions: A multicenter medication reconciliation QI initiative using a refined best practices toolkit was associated with a significant reduction in unintentional medication discrepancies. Future efforts should focus on ensuring as many patients as possible receive effective interventions to minimize discrepancies.