Background: Transitions of care are critical to maintaining patient safety and decreasing adverse events, but they remain a complex process with many pitfalls. Electronic Medical Record (EMR) based handoffs can enhance communication by centralizing content for serial handoffs between providers, facilitating real-time updates and automatically incorporating patient data elements. Over the past several years, much of the literature has focused on the development and implementation of standardized trainee sign-out systems. However, there is a paucity of data demonstrating the effect of standardized EMR based sign-out on hospitalist efficiency and experience.
Purpose: This study aims to evaluate how EMR based sign-out impacts hospitalist satisfaction and efficiency.
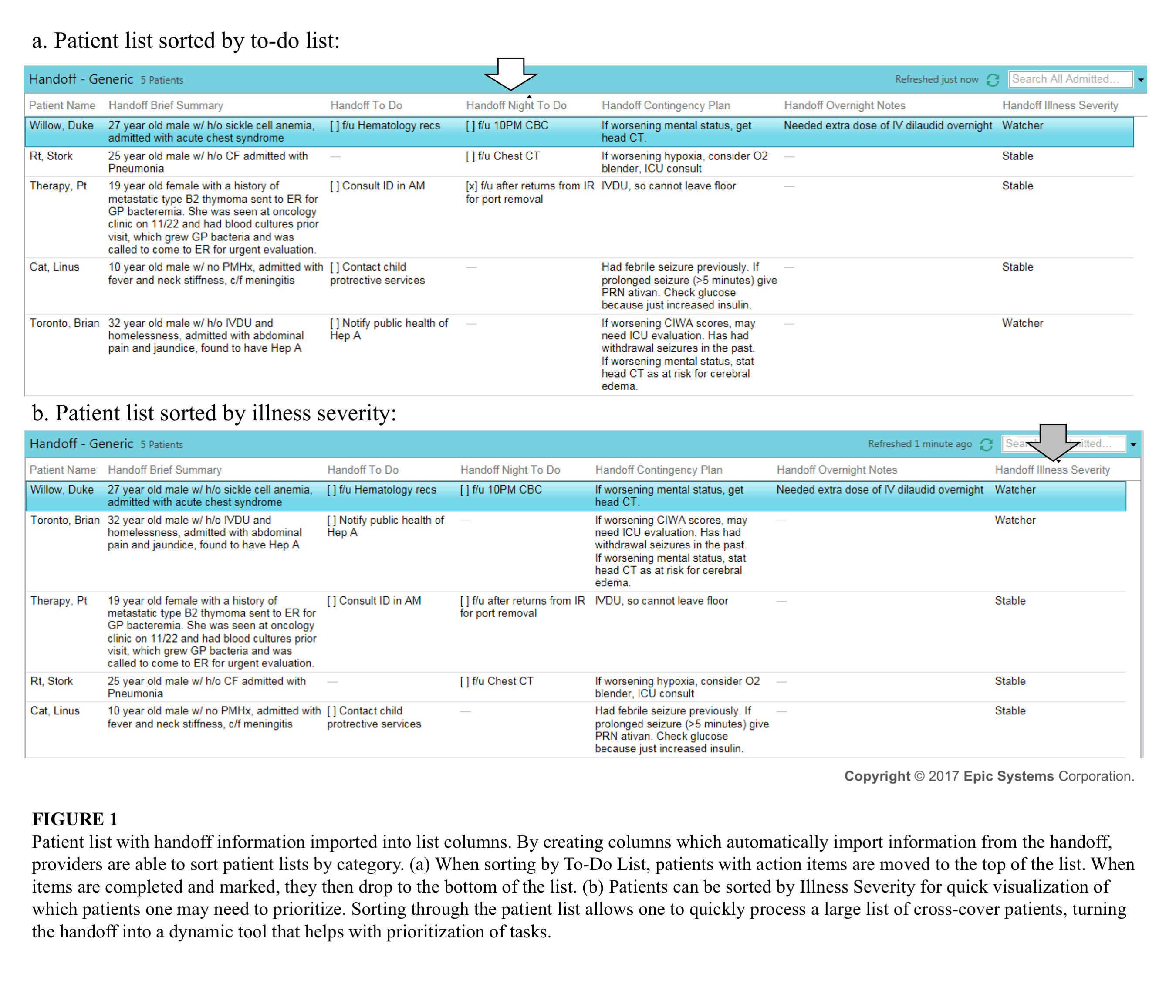
Description: This is a retrospective pre- and post-intervention cohort study. Prior to implementation an email survey was sent to forty hospitalists with thirty-nine respondents. About 75% of those who responded had a hybrid shift-mix of days and nights, and the remaining 25% were either exclusively daytime hospitalists or nocturnists. The group of respondents encompassed a wide range of experience levels from early to late career hospitalists. We then transitioned from an e-mail based free text style sign-out to a standardized EMR based handoff system. Data elements included an assessment of clinical illness severity, patient summary, active problems, overnight to-do list, cross-cover updates and a day-time hand-off to do list. Four months after EMR handoff implementation the same group of hospitalists was re-surveyed. All thirty-nine hospitalists completed the survey. Chi-square tests were used for statistical analysis. There was a significant increase in the number of hospitalists who reported that the sign-out method was an efficient use of their time (10% pre-implementation vs. 59% post-implementation, p<0.000001). This was supported by reported time spent on weekly switch day sign-out. Prior to implementation of the EMR handoff tool, 70% of hospitalists reported spending >45 minutes on weekly switch day sign-out versus 45% post-implementation (p= .025). There was no significant change in self-reported sign-out accuracy with EMR handoff implementation (p=0.25). Overall, the number of respondents reporting general satisfaction increased from 54% to 82% (p<0.009). In addition to improving efficiency and satisfaction, our tool offers other advantages including easy access to sign-out from within the patient chart and the ability to incorporate sign-out elements into patient lists which can then be sorted by illness severity, cross coverage notes and incomplete follow-up tasks (shown in Figure 1).
Conclusions: This study aimed to evaluate EMR based sign-out on hospitalist efficiency and satisfaction. The data shows that standardization of an EMR sign-out tool is an opportunity to improve hospitalists’ work-flow. While our study suggests that changing to EMR based sign-out does not influence accuracy, it is uncertain how this system change impacts patient safety. Future directions of study include integration of calculated clinical illness severity scores and linking hand-off innovation to improved clinical outcomes.