Background: In shared decision making models, decisional conflict is a measure of uncertainty and readiness and comfort level in making a decision. The literature examining decisional conflict is currently relatively immature. The act of a patient being readmitted is, in part, an effect of multiple small decisions a patient makes in the time between index hospitalization, discharge, and readmission. An understanding of how patients interact with the healthcare system and why certain choices are made by patients, is a crucial body of knowledge for all who are working to improve healthcare delivery to understand.
Methods: Daily admission and estimated date of discharge data was obtained via a daily report for the general medicine service at Ronald Reagan UCLA Medical Center. Patients were then screened for exclusion criteria by contacting the charge nurse of the patient’s unit. Trained quality improvement team members approached all remaining patients who were being discharged from the general medicine service within 48 hours and assessed for willingness and ability to participate.
Decisional conflict was measured using the SURE tool, a validated 4-item tool that has been shown to have adequate psychometric properties in assessing for the presence of decisional conflict. Patients were asked to “picture the scenario of being discharged from the hospital and in the subsequent days not feeling well.” They were then asked to answer the following questions: “to seek medical attention, would call your primary care provider or specialist, go to the emergency room, go to urgent care, or wait for your scheduled follow-up appointment?”. The SURE tool was scored and a decisional conflict was considered positive if any 1 of the 4 questions was marked as “no.”
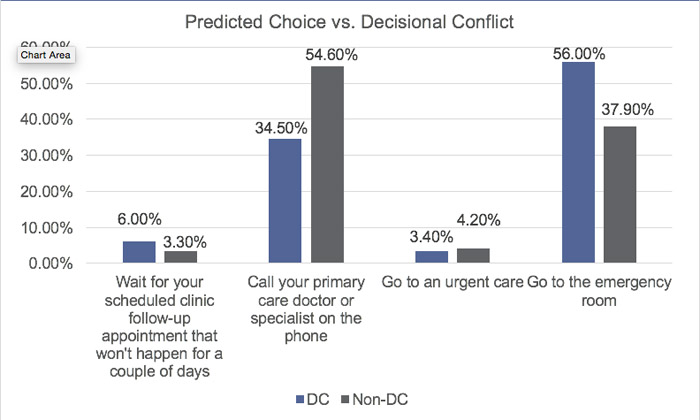
Results: In our initial pilot data, a total of 422 patients were evaluated for decisional conflict. 116 patients (27.5%) tested positive. Significant associations, p<0.05, for decisional conflict included: patient location (unit), age, and predicted choice. Conflicted patients were older (62 years of age vs. 57). Conflicted patients were significantly more likely to decide to seek the emergency room for their post-hospitalization care and less likely to call their PCP or specialist (65 (56%), vs 40 (34.5%)). When holding the Choice and Unit constant, likelihood of decisional conflict increases by 2% with each additional year of age (P<0.05). Regression analysis demonstrated that patients on the general medicine floors were 51% less likely to be conflicted when compared to patients in the “Other” Unit category. Pilot data did not demonstrate a significant association between decisional conflict and 30-day readmissions rate (24.3% vs. 22.5% for conflicted and non-conflicted, respectively); however, the study was underpowered to do so.
Conclusions: Our findings suggest that patients with decisional conflict may make different choices about their post-hospital follow-up care in comparison to patients without decisional conflict. Furthermore, there may be operational associations – boarding patient status – that have a significant impact on patients having decisional conflict surrounding their post-hospital care. Educational interventions on index discharge to promote contact with PCP/specialists for patients who test positive for decisional conflict to enable them to better navigate the outpatient healthcare resources may decrease ER utilization. Finally, standardized training across all units may impact decisional conflict amongst patients on boarding units.