Background: Effective teams share common attitudes, behaviors, and cognitions that support teamwork. Within patient safety literature, effective teamwork is a core feature of interventions that reduce adverse events. However, research on teamwork in healthcare has focused on teams of healthcare professionals and has not examined how patients and their family caregivers experience teamwork as part of health care. The aim of this study is to explore the facilitators and barriers to effective post-discharge teamwork between older patients with heart failure, their family caregivers, and the medical team from the perspective of patients and their family caregivers.
Methods: We conducted a qualitative study of patients and caregivers, recruited during a hospital admission at a tertiary referral hospital. Eligible patients were 65 years of age or older, were admitted with a principal diagnosis of heart failure, had a primary care provider they had seen in the past year, and were discharged home. Caregivers were identified by the patient. Patients and caregivers completed independent interviews 30 to 60 days following discharge. Interviews were recorded and transcribed verbatim. The semi-structured interview guide elicited patient and caregiver perceptions on post-discharge goals, team membership, team leadership, team communication, and roles and responsibilities. We completed a directed content analysis using a framework of attitudes, behaviors, and cognitions of effective teamwork from Industrial and Organizational Psychology.
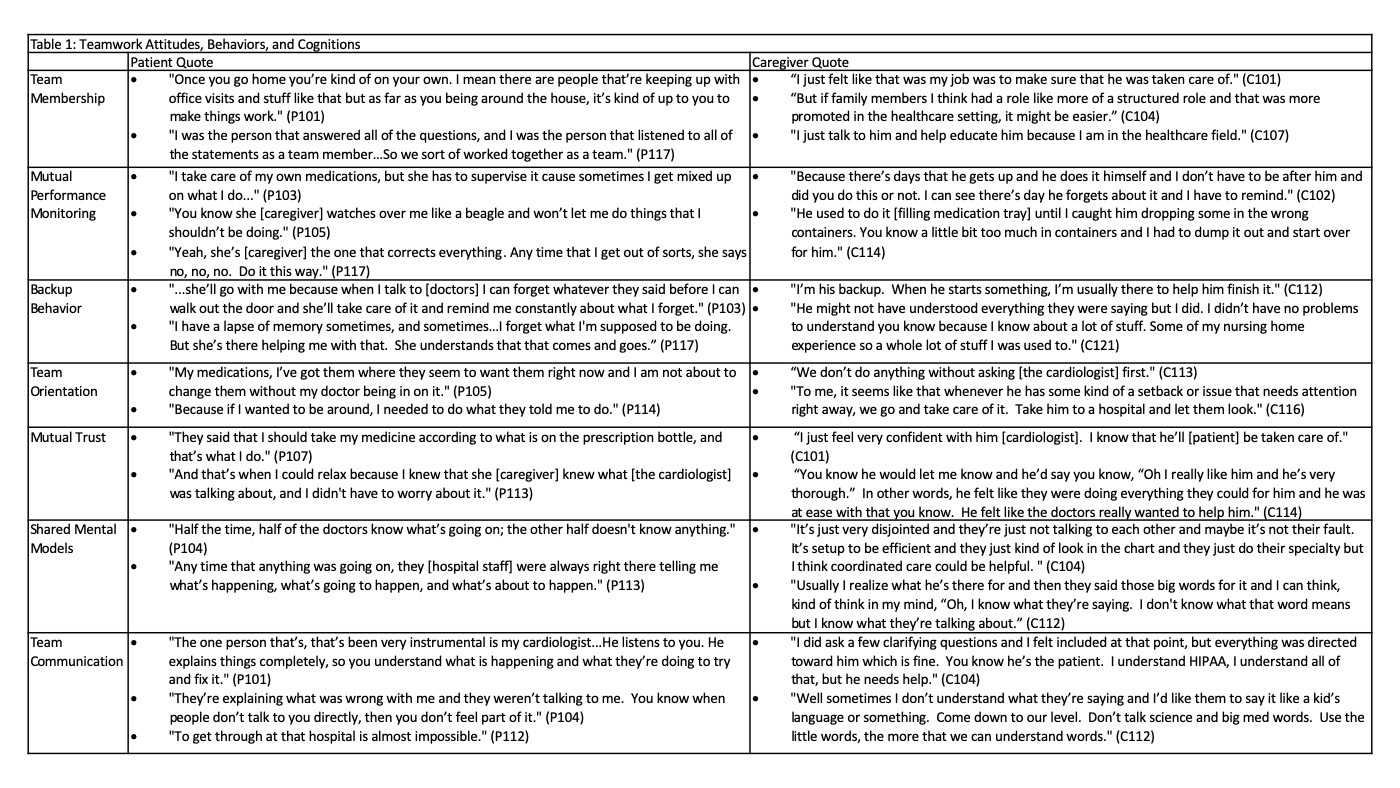
Results: Fifteen patient and fifteen caregiver interviews were completed (n=30). The average age of the patients was 72 years (range 65-90). Caregivers were spouses (n=12), adult children (n=2), and a roommate (n=1). Representative quotes are provided in Table 1. Patients and caregivers reported a range of individuals who they considered to be members of their post-discharge team including, inpatient physicians and staff, outpatient physicians and staff, home health providers, family, friends, and neighbors. Patients and caregivers reported understanding their own roles and responsibilities following discharge; however, many identified these roles and responsibilities independently without discussion with other team members. Only six dyads agreed on who was the team leader (caregiver n=2, cardiologist n=2, primary care provider n=1, and inpatient physician n=1). Although patients expressed concern about “losing their independence”, patients and caregivers accepted the need for caregivers to monitor patient actions and provide backup when needed. Patients and caregivers were receptive to feedback from providers and trusted their advice; however, patient and caregiver experiences communicating with providers was mixed and impacted their understanding of how team members would interact.
Conclusions: Conclusions: Following hospital discharge, patients and caregivers work within teams that include healthcare providers, family, and friends. Although critical to ensuring the safety and quality of care transitions, clear delineation and agreement of team member roles and responsibilities, team leadership, and an understanding of how team members will interact are often missing. Although the challenges of communication with providers following discharge has been well described, this study adds to our understanding of the specific areas in which better communication could improve team function.