Case Presentation: A 63-year-old man with history of recurrent syncope and atrial fibrillation (AF) on warfarin presented to our hospital with headache. Within the last year, he had suffered several falls due to syncope, which resulted in serious injuries, including jaw fracture and subdural hematomas (SDH). He used alcohol and marijuana daily. Previous workup for seizure activity, orthostatic hypotension, and vestibular dysfunction was negative. A recent Holter monitor showed 0.4% AF burden and rare supraventricular tachycardia. On our exam, the patient had regular heart rhythm, with no orthostatic changes or focal neurologic deficits. Laboratory findings were remarkable only for an international normalized ratio of 4.9. CT head did not show any pathology.
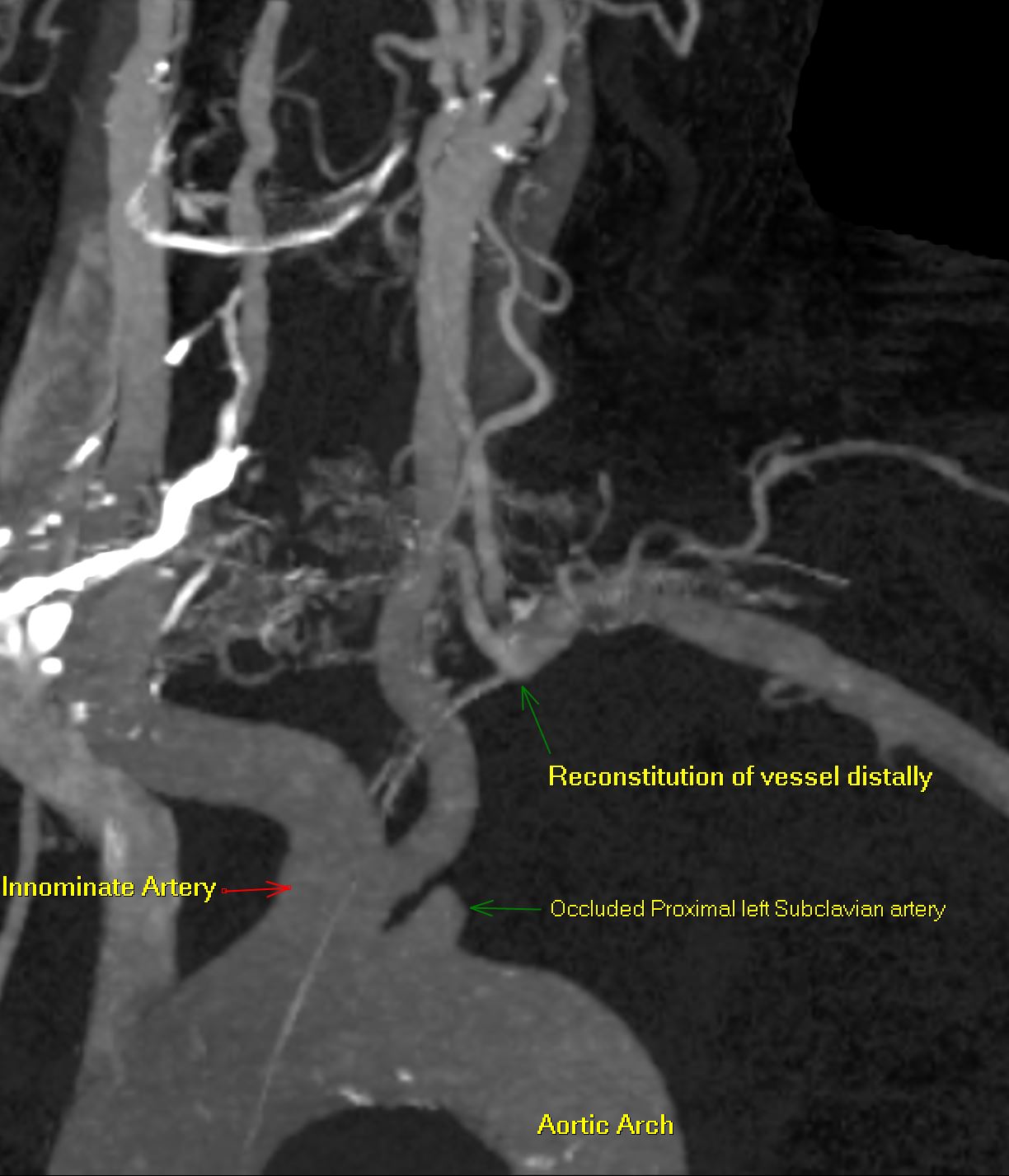
Review of his medical record revealed a prior carotid ultrasound showing retrograde flow in the left vertebral artery, raising suspicion for subclavian steal syndrome (SSS). On further questioning, he disclosed that minimal exertion (e.g., unloading a few items from dishwasher) caused left arm pain and paresthesias, accompanied by headache and lightheadedness. Interarm systolic blood pressure (BP) difference of >40 mmHg was found, and left arm claudication was reproducible. CTA neck demonstrated total occlusion of the left proximal subclavian artery and patent bilateral internal carotid arteries. Revascularization was deferred until further evaluation of arrhythmia and substance use, in order to rule out these potential causes of syncope. A month later, the patient sustained more falls with vertebral fractures at C1, C4, and L1, as well as SDH requiring bone flap/clot evacuation. An event monitor revealed many syncope events without arrhythmia. He later died in neurology intensive care unit.
Discussion: SSS results from steno-occlusion of the proximal subclavian artery with subsequent retrograde flow in the ipsilateral vertebral artery. SSS is usually asymptomatic but can present with vertebrobasilar and brachial symptoms, including dizziness, syncope, ataxia, arm claudication, and paresthesias. Diagnosis is made by careful history, exam, and imaging. Symptomatic patients often have additional disease in anterior vasculature (e.g., carotid stenosis), causing inadequate collateral circulation. Our patient suffered symptoms of cerebral ischemia due to subclavian steal, despite having patent carotid arteries. SSS is managed with atherosclerosis risk reduction. Endovascular or open revascularization is reserved for refractory symptoms and has a high success rate with low morbidity. Arm BP discordance >40mmHg correlates highly with the need for intervention.
Conclusions: In a patient with recurrent syncope, SSS should be included in the differential. Symptomatic SSS can occur despite patent carotid arteries. Clinicians should determine the urgency of revascularization in SSS based on clinical symptoms and signs, particularly arm BP discordance.