Background: Hospitalization identifies patients who are particularly costly to the Medicare system and current policy efforts to reduce costs focus on the 30 days after discharge; however, much less is known about which patients will have the greatest long-term Medicare costs. Given the prevalence of functional impairment in Medicare seniors and impact on clinical outcomes of hospitalization, we hypothesized that functional impairment would be a major driver for costs of care up to a year after discharge.
Methods: We studied 7,854 Health and Retirement Study (HRS) subjects who were hospitalized at least once from 2000-2010 (18,598 hospitalizations). Our outcome was total post-acute costs for up to 365 days after hospital discharge, assessed by Medicare claims and adjusted for inflation. Main predictor was functional limitations as determined from the HRS interview immediately before the hospitalization and stratified into 3 levels: no functional impairments, dependency (need for help) in 1-2 Activities of Daily Living (ADLs), and dependency in ≥3 ADLs. Adjustment variables included age, race, gender, income, and net worth (obtained from HRS) and comorbid conditions (Elixhauser calculated from Medicare claims), and prior history of admission. We performed descriptive statistics and multivariable regression analysis adjusted for clustering at patient level to characterize the association of functional limitations and post-acute costs of care.
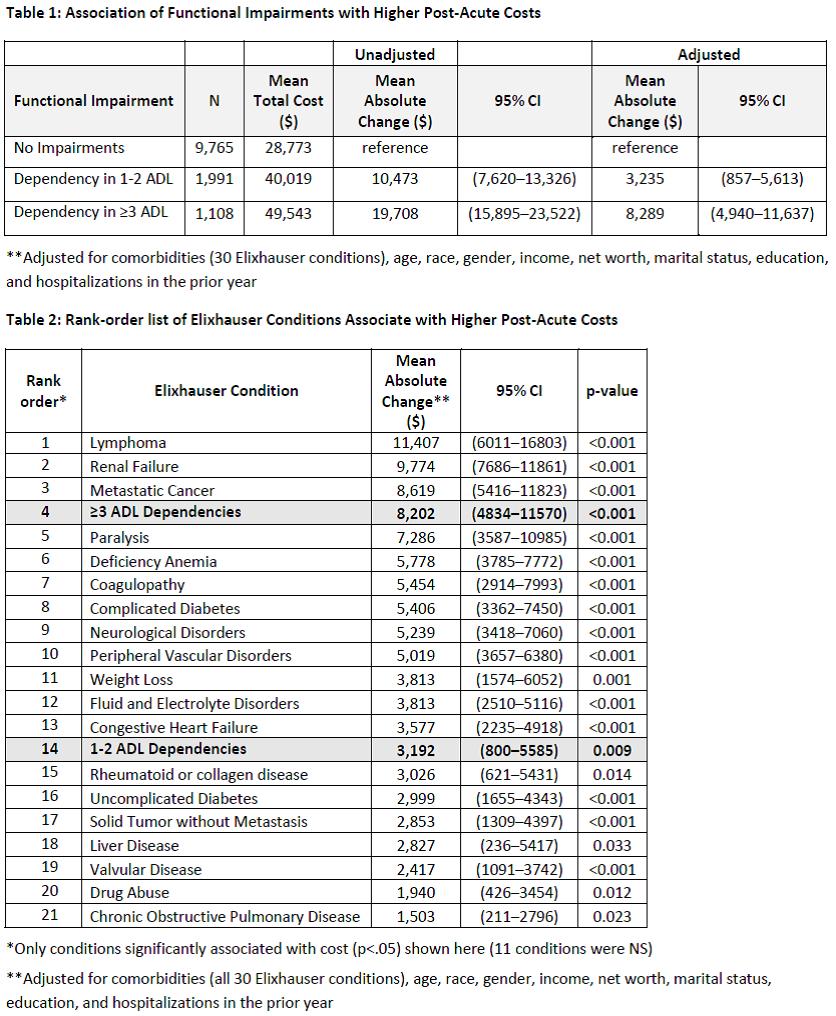
Results: Mean age was 78 (65-105), 44% male, 77% White, 90% reported ≥3 comorbidities, 61% with ≥1 hospitalization in previous year; 48% had had some level of functional impairment prior to hospital admission. Adjusted analyses suggest that patients with more severe impairments have much higher post-acute costs at 1 year: those with 1-2 ADL dependencies cost $3,235 more (95% CI $857-5,613) and those ≥3 ADL dependencies cost $8,289 more ($4,940-11,637) compared to those with no impairment (Table 1). Relative to other clinical conditions, severe functional impairment is very expensive: we rank-ordered adjusted costs of 30 conditions in the Elixhauser scale and found ≥3 ADL dependencies was #4 behind only Lymphoma, Metastatic Cancer, and Renal Failure. 1-2 ADL dependencies was ranked #14 while CHF ranked #13, Uncomplicated Diabetes DM was #16, and COPD was #21 (Table 2).
Conclusions: Functional impairment is associated with significantly higher post-acute costs in Medicare seniors; severe impairment is one of the most expensive conditions in this population. Our findings suggest the need for Medicare policy to expand beyond the traditional focus on chronic disease management and explore initiatives to manage functional impairment in order to reduce overall costs of care for community-dwelling seniors.