Background: In most hospitals, physicians provide care to patients across multiple units while nurses are often unit-based, resulting in team dispersion, and potentially impairing teamwork. Geographically localized care teams may demonstrate improved communication between team members and with patients, potentially enhancing coordination of care. However, the impact of geographically localized teams on patient experience scores is not known. At our hospital, medicine house-staff inpatient teams have a designated “home unit” with office space for charting, team meetings, teaching, communication and coordination of care. When logistically possible, patients cared for by a given housestaff team are assigned to that team’s “home unit”, but patient flow constraints result in some patients residing on a non-home unit. We aimed to assess patient perceptions of care when cared for on the home unit (“geographically localized” patients) versus non-home unit (“off-unit” patients).
Methods: We conducted a retrospective analysis of 10-year patient level HCAHPS data, linked to administrative data, for a single academic tertiary care hospital. Multivariable logistic regression, adjusting for age, sex, LOS, severity of illness, was used to examine the association between geographic localization and percent top-box HCAHPS scores. A sub-group analysis for a 44-month period was conducted, during which multidisciplinary rounds were started and focused efforts resulted in much higher patient localization. This was called the “increased localization period”.
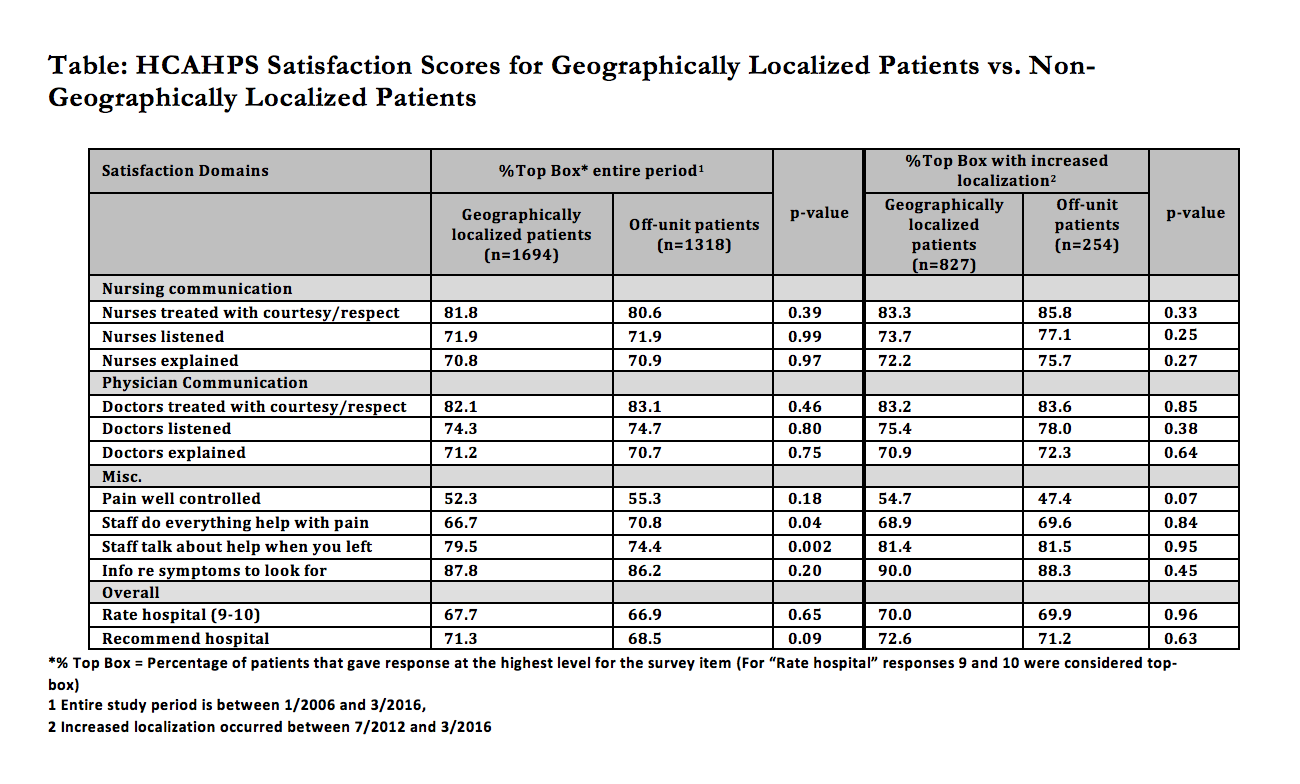
Results: There were 3012 patients in the study and 56.2% of them were localized. During increased localization period, 76.5% of the patients were localized. Patients on localized teams more often perceived that the staff provided information about symptoms to look for at home (79.5% vs 74.4% p=0.002), but patient experiences were similar on all other domains. This did not change during the increased localization period.
Conclusions: Surprisingly, patients cared for by geographically localized teams did not have enhanced patient experience. Other factors like physician communication skills or limited time spent in direct care may overshadow the impact of team localization. Whether focused interventions that take advantage of physician proximity to patients through augmented patient-physician communication (e.g. evening patient rounds on complex patients) might enhance patient experience deserves further study.