Background: Nosocomial infections are one of the leading causes of mortality and morbidity in the United States. Approximately two million people annually are affected by nosocomial infections in the United States and about 80,000 deaths occur each year. Transmission of healthcare associated infections occurs most often by contaminated hands of health care personnel. Hand hygiene has been one of the most effective interventions to prevent nosocomial infections. Despite readily available and easily performed, the adherence rates amongst providers per previous research has been below 50%.
Methods: We conducted observational study in an inpatient setting where hand hygiene compliance was monitored on hospitalist floor in the month of October 2018. Variables collected in the survey include: gender, type of health care personnel, hand hygiene performed or not, if not performed then when was it missed (entry, exit, or both) and possible reasons for not performing hand hygiene. Prevalence of hand hygiene was analysed in overall sample and stratified by gender and healthcare personnel. Significant differences between groups were ascertained by maximum likelihood ratio. SAS 9.4 was used for data analysis.
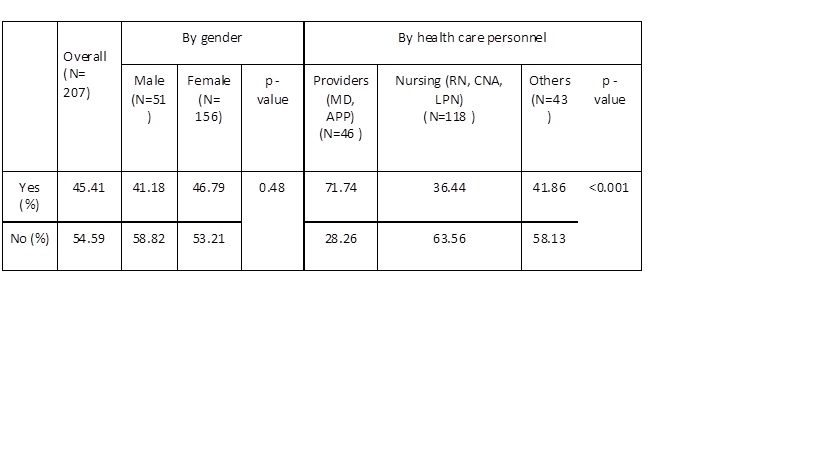
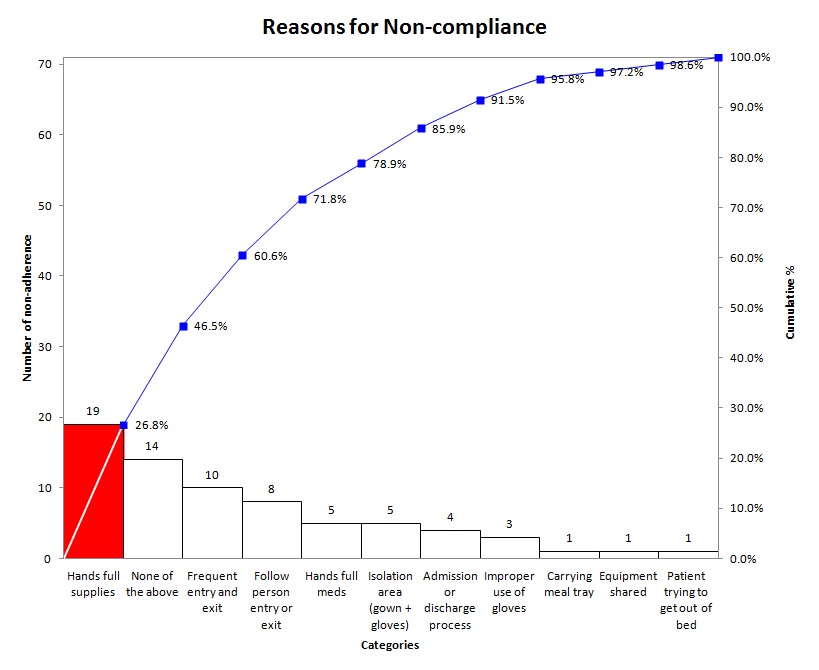
Results: 207 personnel were randomly and anonymously observed. 54.6% of study personnel did not comply with hand hygiene, out of them 43.3% failed to perform hand hygiene at both entry and exiting patient’s room, 46.9% at entry and 9.7% at exit. Prevalence of non-compliance was similar among male (58.8%) and female (53.2%) (p-value 0.48). Only 28.3% providers (MD and APP) found to have non-compliance to hand hygiene compared to 63.5% in nursing and 58.1% in other personnel (p-value <0.001). Hands full supplies or medicine and frequent entry and exit were two top reasons for non-compliance (33.8% and 14.1% respectively). 19.7% did not have any valid reason. Lastly, there was a difference in observation between infection prevention department (70-85%) and our study. The falsely elevated rate in adherence rate from infection prevention department could be due to Hawthorne Effect so subjects would show positive behavior when they know they are being monitored.
Conclusions: Unfortunately majority of healthcare personnel are not performing proper hand hygiene during patient encounter. Non-compliance rate is higher among nursing and other logistic personnel compared to providers (MDs and APPs) and main reason is carrying supplies or frequent exit or entry. Opportunity exists to explore and improve hand hygiene through different intervention.