Background: Academic health systems must balance caring for patients in their community with their role as referral centers for more profitable tertiary quaternary (T/Q) care. Hospital Medicine services, which admit patients largely from the emergency department, often have the lowest proportion of T/Q care and may thus be under pressure to demonstrate their value to the health system. We aimed to determine the composition of patients cared for on our Hospital Medicine service by looking at their previous ambulatory encounters and their connection to the rest of the health system.
Methods: We performed a retrospective review of all patients discharged from our large, urban, Hospital Medicine service from July 1st, 2021 through June 30th, 2022. To determine the connection of these patients to the rest of our health system, we extracted all ambulatory encounters for the year preceding their admission. We excluded encounters that were unlikely to represent a meaningful prior connection to our health care system (e.g. refills, labs, COVID testing and care, and care at affiliate sites). Based on encounter location and our institutional definition of T/Q care, we categorized the ambulatory encounters as primary care encounters, specialty encounters (including procedural encounters e.g. ambulatory surgery, endoscopy, bronchoscopy, interventional radiology), T/Q clinic encounters, and diagnostic services (e.g. echo, radiology, etc.). An ambulatory clinic encounter included only primary care encounters, specialty encounters, and T/Q clinic encounters.
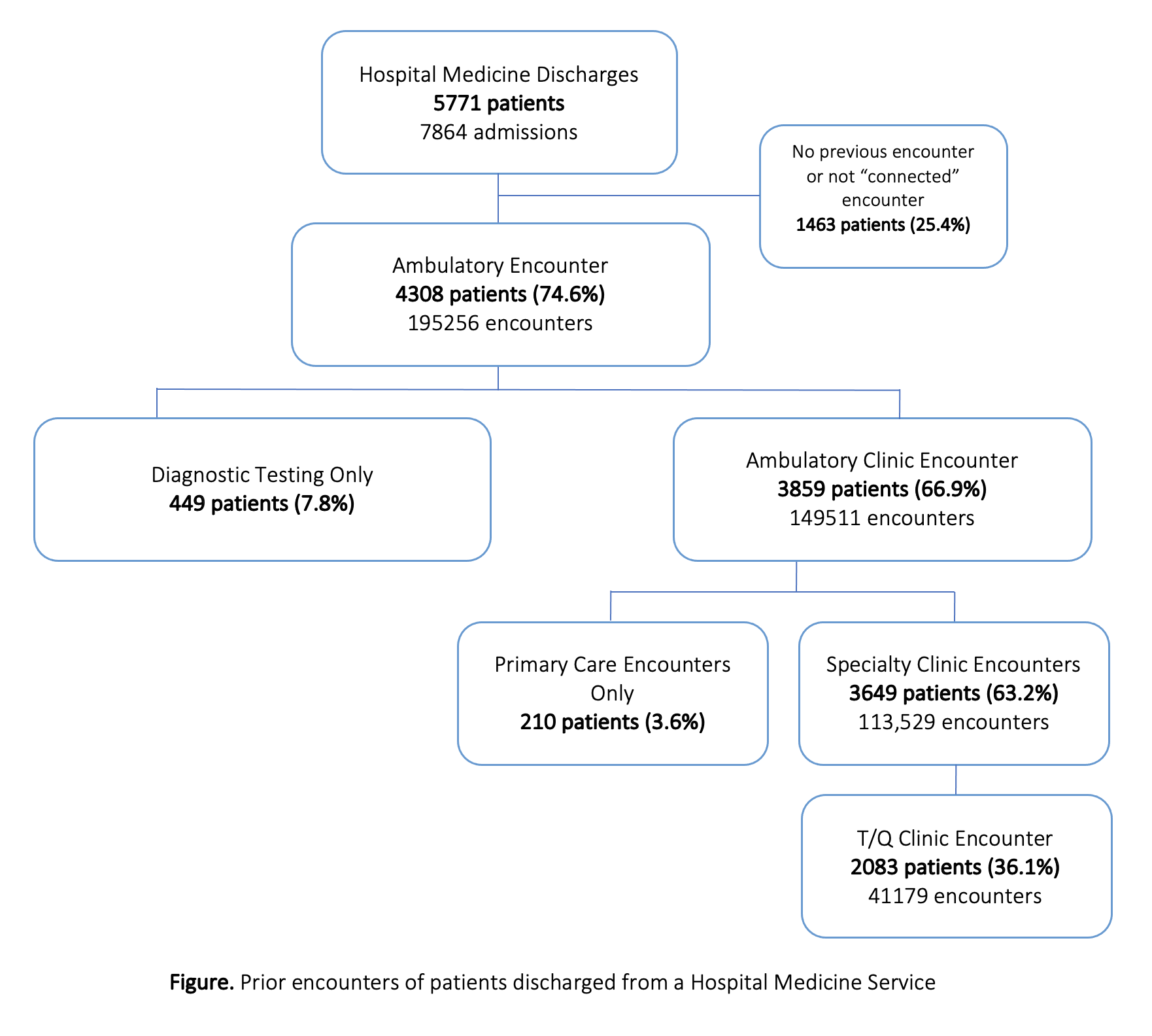
Results: During the study year, 5,771 patients were discharged from the Hospital Medicine service, comprising 7,864 total admissions (Figure). Nearly three quarters (74.6%) of patients had at least one prior outpatient encounter at our institution, with the majority (63.2%) of patients having at least one encounters with a specialist. Only a small fraction of patients only had diagnostic encounters (7.8%) or primary care encounters (3.6%) . While over half of admitted patients received at least one prior diagnostic study at our institution, only 7.8% had diagnostic testing as their only prior ambulatory encounter. Over a quarter of all admitted patients had at least one encounter with our primary care, however only 3.6% of patients had primary care be their sole connection to UCSF. Of the patients receiving outpatient specialty care at UCSF, more than half were of strategic priority to our institution with a prior encounter in a T/Q specialty area.
Conclusions: Our study provides a framework for academic Hospital Medicine services looking to assess their patient population’s connection with the broader health system. We found that 75% of patients cared for by the Hospital Medicine service had a previous encounter in the UCSF network. While only 5% of patients hospitalized on the Hospital Medicine service are categorized as T/Q care, over one-third of Hospital Medicine patients are established UCSF patients with visits in departments of strategic importance to UCSF. This suggests that our Hospital Medicine Service provides inpatient care to a population critical to the role of the institution in our community both locally and regionally.