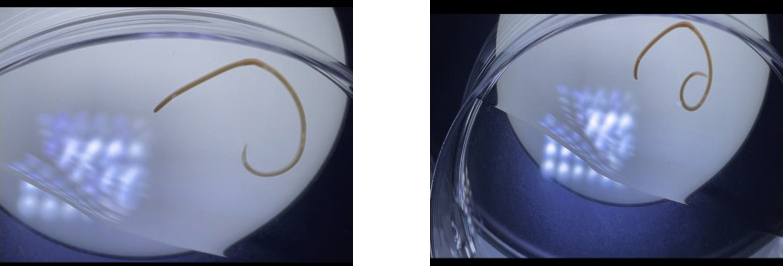
Case Presentation: A previously healthy 19 year-old college student presented after coughing up a live worm (Figure 1). The night prior, he had developed a cough and right-sided chest “cramping.” Although he reported respiratory and constitutional symptoms from his concurrent COVID-19 infection, he stated that the cough was atypical and was associated with a sensation that something was “stuck in the throat.” His symptoms resolved after the expulsion of a live worm. Two days prior to presentation, he had eaten raw salmon sushi with another individual who reported no symptoms. The patient denied walking barefoot along outdoor areas/beaches or having any sick contacts. He did not have emesis, diarrhea, or urinary symptoms. His bowel movements were unchanged, and he had not seen any worms in his stool. Physical examination was unremarkable. Labs including complete blood count and basic metabolic panel were within normal limits. Analysis of the live worm revealed the morphology of Anisakis. The patient was observed for 24 hours without any events, and he was then discharged from the hospital.
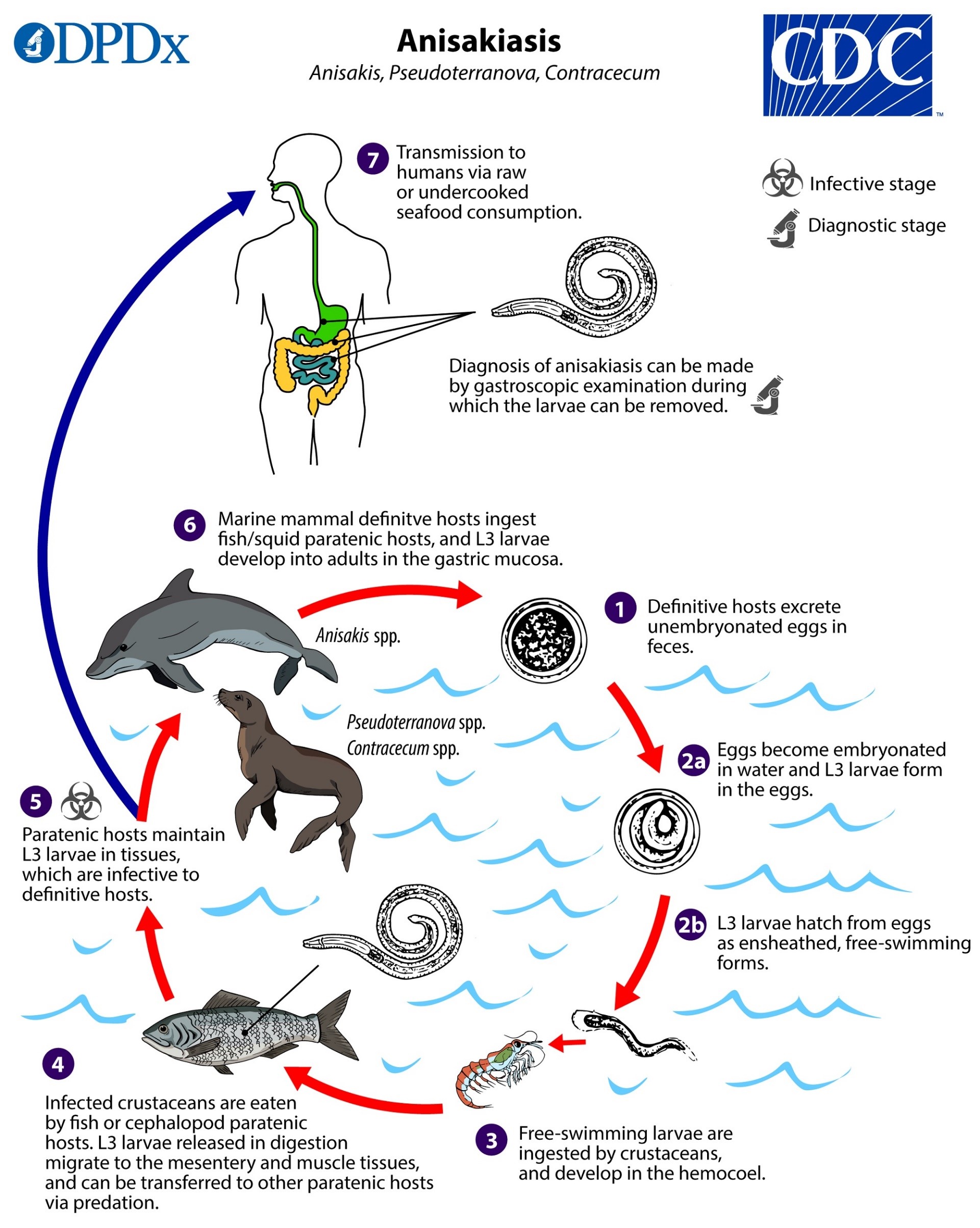
Discussion: Anisakis species are nematodes and an uncommon cause of human parasitic infection. From seawater eggs, they become free-swimming larvae which are ingested by crustaceans, which are then ingested by fish. The larvae burrow into the gut of a fish or other predatory marine mammal where they will grow into adults (Figure 2). Humans are incidental hosts — the life cycle of the worm cannot continue in the human. The prevalence of anisakiasis is highest where raw fish and seafood consumption is common, in particular, Japan, the Pacific coast of South America, and Northern Europe. Anisakiasis is rare in the U.S., and when it occurs, it is more commonly seen in the Southwest including California. Anisakiasis is a self-limited infection with a short course owing to larvae being unable to survive in human hosts. Anisakis can burrow into human intestines resulting in irritation presenting as acute abdominal pain, usually within hours after ingestion. Irritation increases the risk of bowel obstruction. Some individuals develop allergic reactions to the worm and may present with rash, itchiness, and even anaphylaxis. If passed into bowel, a severe eosinophilic granulomatous response may occur 1 to 2 weeks following ingestion characterized bloody or mucoid diarrhea, abdominal pain, vomiting, and potential intestinal perforation. Our patient brought in the live worm. Diagnosis requires histopathologic examination of worm gathered through endoscopy, surgery, or in this case, self-expulsion through regurgitation. Although eosinophilia may hint at a parasitic infection, it is often not present when infection is not systemic. First line treatment is removal of the worm. In some cases, albendazole may be prescribed. Without the worm, a definitive diagnosis cannot be made, but an exposure history could lead to suspicion for anisakiasis. Prevention of anisakiasis relies on cooking and freezing seafood properly to FDA-recommended temperatures.
Conclusions: Anisakiasis is a rare infection in areas with food regulations in place. Exposure history can facilitate the diagnosis with or without the presence of the live worm. Removal of the worm allows for definitive diagnosis and also serves as first line treatment. Observation may be warranted for potential complications. Most infections are self-limited, and symptoms usually resolve after the Anisakis worm is out of the body.