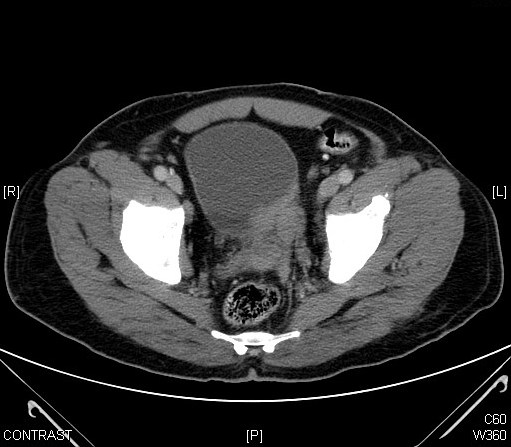
Case Presentation: A 64 yr old gentleman presented to the emergency department of our hospital with abdominal pain and hematuria. Initial laboratory evaluation revealed unremarkable metabolic profile and mild anemia (Hgb -9.3 g/dl). Urinalysis was full of RBC’s with negative culture. CT abdomen revealed bilateral hydroureteronephrosis (HDUN) with a bladder mass (Fig I). Cystoscopy revealed a friable mass at the dome of the bladder extending to bilateral ureteral orifices and a biopsy from the mass showed small to intermediate blasts with flow cytometry positive for CD10, CD34, CD19, TDT, CD38 and CD45. Bone marrow biopsy was significant for 100% cellularity with absent trilineage hematopoiesis and almost complete effacement of the marrow by blasts which were positive for CD10, CD34, CD19, TDT, cytoplasmic C79a, CD38, HLA-DR and CD45. The patient had bilateral ureteric stents placed for worsening acute kidney injury (AKI) in addition to HyperCVAD therapy (fractionated cyclophosphamide, vincristine, doxorubicin and dexamethasone). Following four cycles the patient achieved complete remission with repeat BM showing evidence of trilineage hematopoiesis and 3% blasts on a 100 cell count and repeat CT imaging revealing resolution of the bladder mass (Fig II).
Four months later he underwent surveillance cystoscopy revealing negative for leukemia but positive for new prostate adenocarcinoma. In view of his large volume prostate (44.5 gm) and locally advanced disease he was treated with a combination of external beam radiotherapy (EBRT) and androgen deprivation with leuprolide. Following radiotherapy, he started his maintenance therapy with 6-MP (mercaptopurine), PO and intrathecal methotrexate and vincristine. Persistent pancytopenia obligated reduction of dosage to 25% of the total dose.
Currently, >2 years later patient is well in complete remission.
Discussion: Neoplastic infiltration of the genitourinary tract in adults is more commonly reported to the kidneys. Suriya OM et al reported two patients with hematuria but in both cases biopsy proven leukemic infiltration could not be demonstrated. We report a unique situation with an adult patient with hematuria and a bladder mass and biopsy proven leukemic infiltration.
Bladder metastasis are of two types infiltrative (diffuse) and proliferative (protuberant), with proliferative being the more common pattern. In a review of 282 cases of metastases to the urinary bladder from distant foci reported since 1953, melanoma followed by gastric and breast were the most common primary sites. No cases of leukemia were identified though 4 patients with lymphoma were diagnosed post-mortem with bladder metastases. Although the exact mechanism remains elusive, hematological and lymphatic spread remains the widely proposed hypothesis in leukemic metastases.
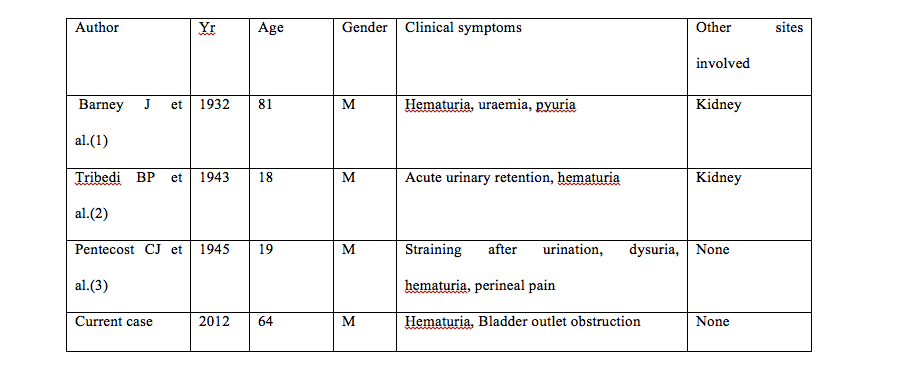
Demographic data on three adult patients with ALL associated bladder metastases is summarized in Table I. Immunophenotyping data on these cases is not available since cytogenetics and risk grouping was not used at the time of their publication.
Conclusions: What makes our case unique is the identification of pre B cell ALL since the risk of organ infiltration may not be uniform across all subtypes. Further, our case demonstrates the importance of index of suspicion since early diagnosis is the key to establishing long term remission in these patients.
Our patient further presented a clinically challenging situation with development of a second malignancy during ongoing therapy for leukemia