Case Presentation: Hemophagocytic Lymphohistiocytosis (HLH) is a rare, inappropriate immune response causing excessive inflammation and multiorgan failure if left untreated. Hereby we present a hematologic case of systemic mastocytosis (SM) and secondary HLH. A 79-year-old female was under evaluation for chronic fatigue and asymptomatic hyperbilirubinemia for 6 months. While she had an unremarkable hepatobiliary work-up, she was found to have anemia with thrombocytopenia. Bone marrow biopsy revealed SM with hematological neoplasm and large aggregates of histiocytes. Molecular testing detected a KIT D816V mutation. The patient also had elevated ferritin, CRP, CXCL9, IL-18, soluble IL-2 levels, and low tryptase levels. A CT scan of the abdomen showed splenomegaly. The patient was treated with steroid taper and transitioned to midostaurin once HLH and SM criteria were met. The patient’s hyperbilirubinemia and cytopenias improved; however, the patient suffered a slow decline and went under hospice care.
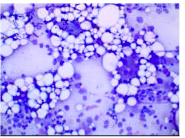
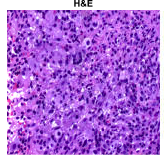
Discussion: HLH is due to abnormal regulation of macrophages, cytotoxic T cells (CTLs), and natural killer (NK) cells. In normal physiological response, macrophages present foreign antigens to CTLs and NK cells which form perforins and release granzyme B; destroying pathogenic antigen-bearing macrophages. In HLH, CTLs are unable to remove macrophages, causing excessive release of cytokines such as interferon-gamma, leading to cytokine storm and multiorgan failure. Macrophages further phagocytose the other three cell lines causing “hemophagocytosis.” Diagnosis of HLH requires 5 of the 9 criteria of the HLH-2004 diagnostic scale: fever, cytopenia affecting at least two cell lines on peripheral blood, ferritin >500 ng/mL, hypertriglyceridemia, hypofibrinogenemia, hemophagocytosis in either bone marrow, spleen or lymph node biopsy, absence or decreased activity of NK cell activity and high levels of soluble IL-2 receptor alpha chain. Our patient met 7 of the 9 criteria for HLH. HLH can be due to a primary or secondary etiology. Our patient was found to have secondary HLH due to SM. Mastocytosis is a process of release and accumulation of mast cells in the skin or multiple organs called SM. Per WHO, diagnosis of SM is made when one major and two minor criteria, or three minor criteria are met: major criteria includes presence of >15% of mast cells in clusters on bone marrow biopsy and minor criteria of tryptase level>20, abnormal CD25 mast cell expression, KIT D816V mutation, or > 25% of atypical mast cells. Our patient met 1 major and two minor criteria. HLH with SM is a rare finding, after literature search, there has been only one other case report with similar presentation. Treatment for SM is limited; however, symptomatic treatment includes trigger avoidance, steroids, and antihistamines. Midostaurin is an approved drug for SM.
Conclusions: Timely recognition of HLH and treatment of underlying cause has shown improved outcomes and patient survival.