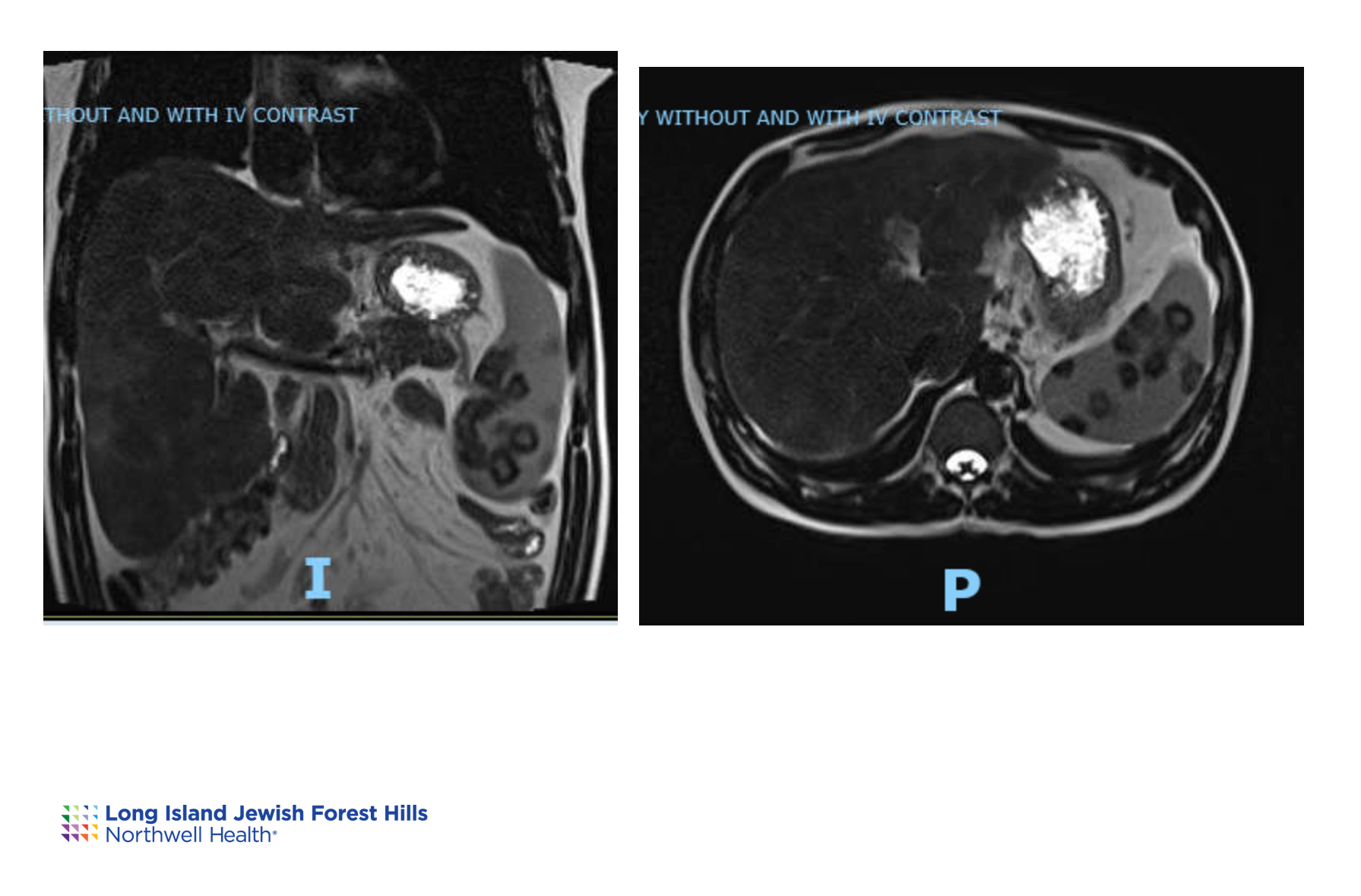
Case Presentation: A previously healthy 32-year-old man presented to the ER for two weeks of yellowing skin and eyes. He denied recent illness, weight loss, GI symptoms, hemoptysis, and night sweats. He had arrived in the US four months earlier after a month-long trek through seven countries. He denied any animal bites, but did drink river water. He was born in Venezuela and grew up in the city. He denied any history of or exposure to TB or harsh chemicals. He worked as a mechanic. He was monogamous with his wife and had no pets. He reported occasional alcohol use but denied using drugs. He had several tattoos. He denied any use of medications or herbal supplements except Vitamin B complex. Physical exam was only positive for jaundice and scleral icterus. A complete blood count with differential and basic metabolic panel were within normal limits. Liver enzymes were elevated in a cholestatic pattern. Inflammatory markers and serum ACE were also elevated. Flow cytometry was negative for findings indicative of lymphoma. Quantiferon, HIV, HSV, CMV, EBV, a full hepatitis panel, blood cultures, urine cultures, stool cultures, stool PCR and O&P, malaria smear, leptospirosis serology, auto-antibodies, and ANCAs were all negative. Imaging described numerous ill-defined nodules predominantly in the upper lung and perilymphatic distribution; retroperitoneal lymphadenopathy; small esophageal varices; numerous ill-defined osteolytic lesions; a cirrhotic liver with confluent hepatic fibrosis; and splenomegaly with lesions throughout.Endoscopic ultrasound-guided biopsy of the liver and lymph nodes found extensive noncaseating granulomatous disease with portal and parenchymal involvement. Also seen were rare asteroid bodies. Samples were sent to the CDC to rule out leishmania, which was negative. AFB stains were negative, and GMS stain was negative for fungal forms. The imaging and biopsy findings, elevated ACE level, and lack of other clear etiology led to a diagnosis of sarcoidosis. He was started on prednisone, and within 2 months his bilirubin and LFTs were back to baseline.
Discussion: Sarcoidosis is a difficult diagnosis to make because of its heterogeneous presentation that may involve any organ system. Diagnosis is usually suspected in those with persistent cough and dermatologic, eye, and lymph node involvement. While our patient had extensive granulomatous findings, his only presenting symptom was jaundice, a clinical sign found in less than 5% of patients with sarcoidosis. Additionally, only 6-8% of patients with sarcoidosis develop cirrhosis. ACE is elevated in only 75% of patients, and liver enzymes are elevated in 50-70%. Liver biopsy is the diagnostic procedure of choice for patients with LFT abnormalities and will show non-necrotizing granulomas and often, asteroid bodies. The treatment for sarcoidosis is a long course of steroids, so even with a positive diagnosis, it is imperative to rule out and treat concomitant infection, which steroids can exacerbate.
Conclusions: This case stresses the importance of a diverse team and unconventional approaches when symptoms don’t align with the expected diagnosis. Jaundice, a rare standalone symptom in sarcoidosis (< 5%), usually accompanies other signs. Prioritizing infection exclusion was crucial due to the treatment's potential impact on different conditions. This highlights the need for a precise diagnostic process to ensure safe and accurate treatment choices.